Below are some of my high yield notes for the general cardiology board examination focusing on vascular diseases with easily sharable supplemental articles and tables my reference.
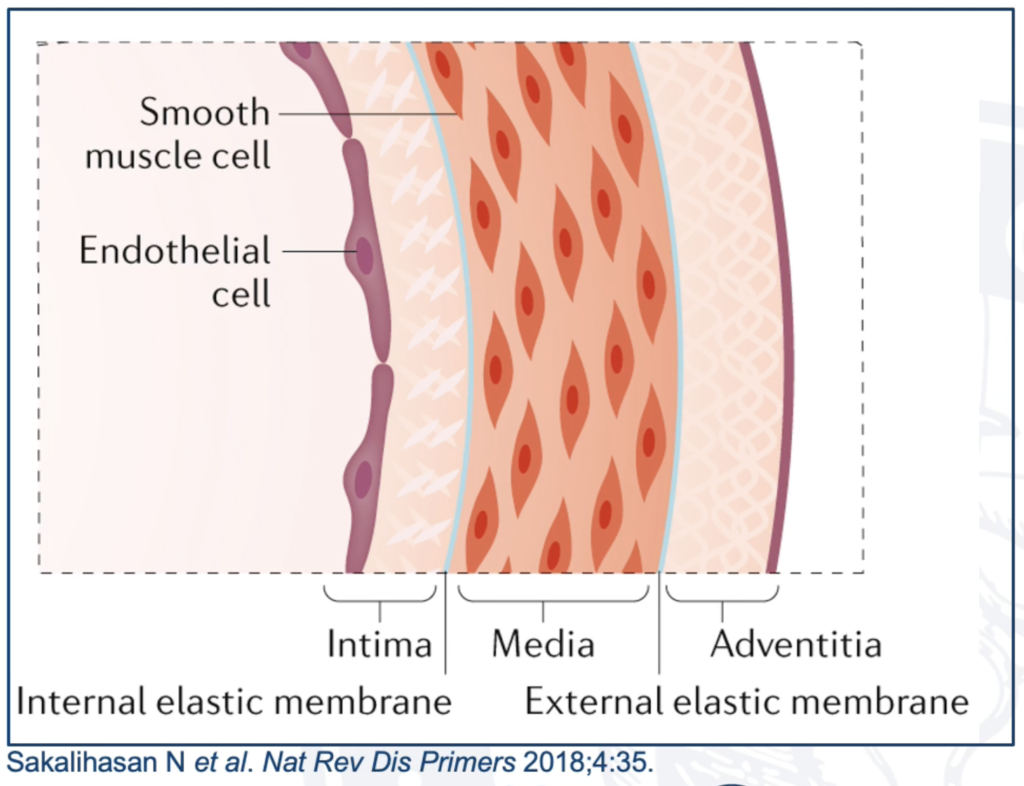
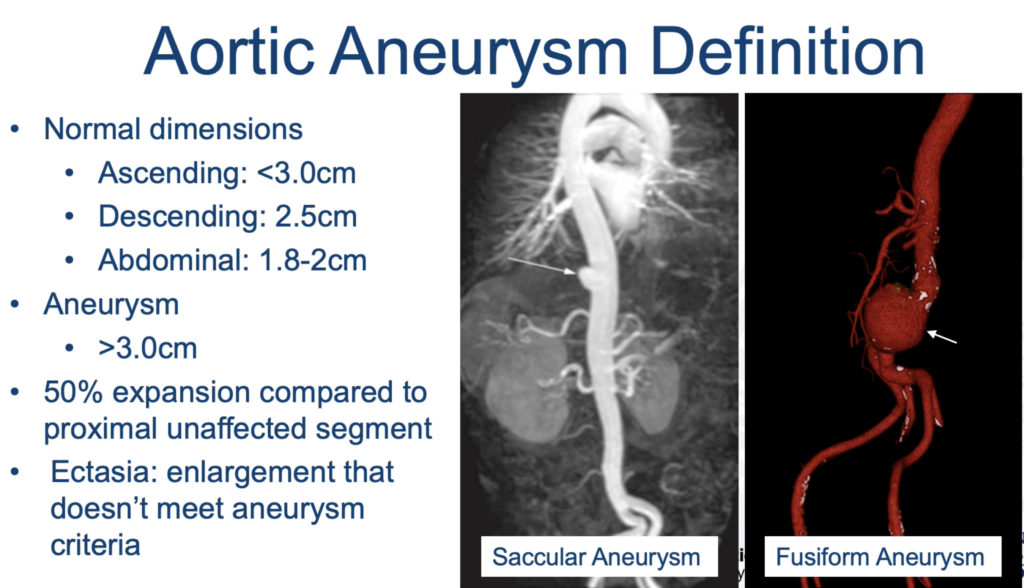
Aortic Aneurysm
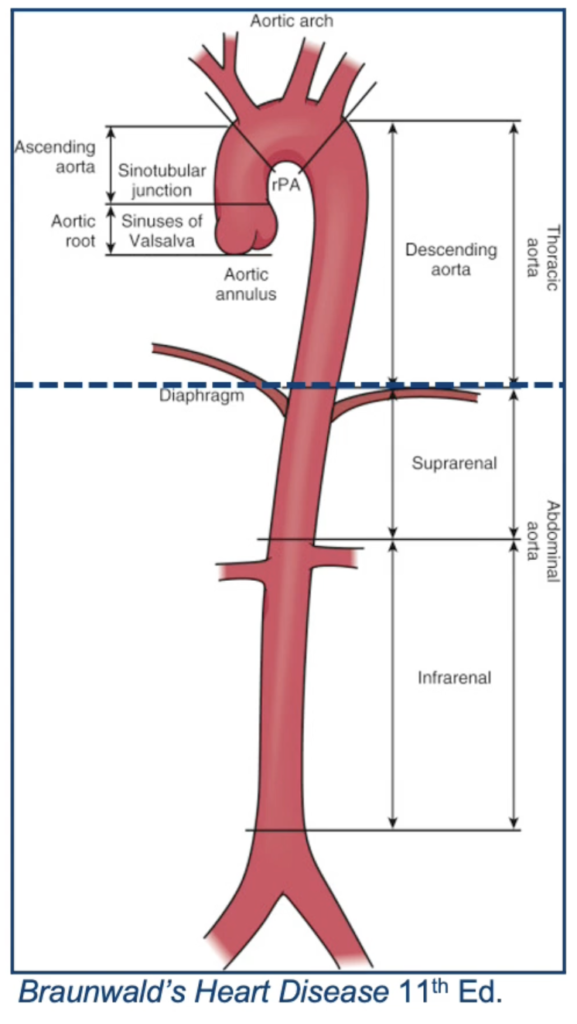
Location:
- Ascending aorta/root: 60%
- Descending aorta: 40%
- Both thoracic and abdominal aorta: 5-10%
Surgical Indications for Thoracic Aortic Aneurysm Repair
| Condition | Size Threshold |
|---|---|
| Aneurysm | ≥5.5 cm |
| Bicuspid AV (BAV) | ≥5.5 cm |
| BAV with risk factors + low surgical risk | ≥5 cm |
| BAC with AVR | >4.5 cm |
| Marfan syndrome | ≥5 cm |
| Marfan syndrome + risk factors | >4.5 cm |
| Loeys-Dietz syndrome | 4 – 4.5 cm |
| Familial thoracic aortic aneurysm syndromes (TAAD) | 4.5 – 5 cm |
| *Abdominal aortic aneurysm | ≥5.5cm |
| *Abdominal aortic aneurysm | >0.5 in 1 year |
- Patients with infrarenal or juxtarenal AAAs measuring ≥5.5 cm should undergo repair to eliminate the risk of rupture. (Level of Evidence B)
- Infrarenal or juxtarenal AAAs measuring 4.0 to 5.4 cm in diameter should be monitored by ultrasound or computed tomographic scans every 6 to 12 months to detect expansion. (Level of Evidence A)
US Screening for Abdominal Aortic Aneurysm
| Patient | Level of Evidence |
|---|---|
| Men 65-75 who have ever smoked | B |
| Men 65-75 who never smoked | C |
| Women 65-75 who have ever smoked | I |
| Women who never smoked | D |
*C: selectively offer given moderate certainty of small benefit
*D: no net benefit or possible harm
I: insufficient evidence
Surveillance Imaging in Known Aortic Aneurysm
| Abdominal Aneurysm Size | Frequency |
|---|---|
| 25-29 mm | 4 years |
| 30-39 mm | 3 years |
| 40-44mm | 2 years |
| *≥45 mm | Yearly |
*Yearly in both thoracic and abdominal aneurysms if ≥45mm. Otherwise repeat thoracic imaging q2-3 years
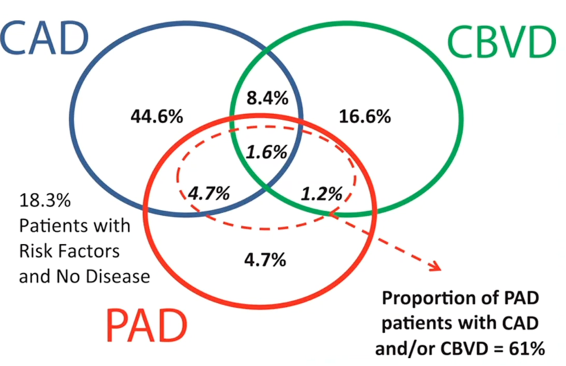
Peripheral Vascular Disease
- Risk factors and odds ratio (95% CI): CAD/CVD 2.27, smoker 2, former smoker 1.87, DM1 1.68, HTN 1.47, age 1.39
- Clinical Presentation of PAD (i.e. angina of the legs): 50% asymptomatic, 33% atypical limb symptoms, 15% typical intermittent claudication, 2-3% critical limb ischemia
- Patients at risk of PAD who should be screened (IIa rec): (1) age ≥65yo, (2) Age 50-64 with risk factors (DM2, smoking history, HLD, HTN) or FH of PAD, and (3) age <50 with DM2 and 1 additional risk factor for atherosclerosis
| Location of claudication | Location of disease |
|---|---|
| Calf | Femoral-popliteal ±aorto-iliac |
| Buttock & calf | Aorto-iliac |
| Buttock | Internal iliac |
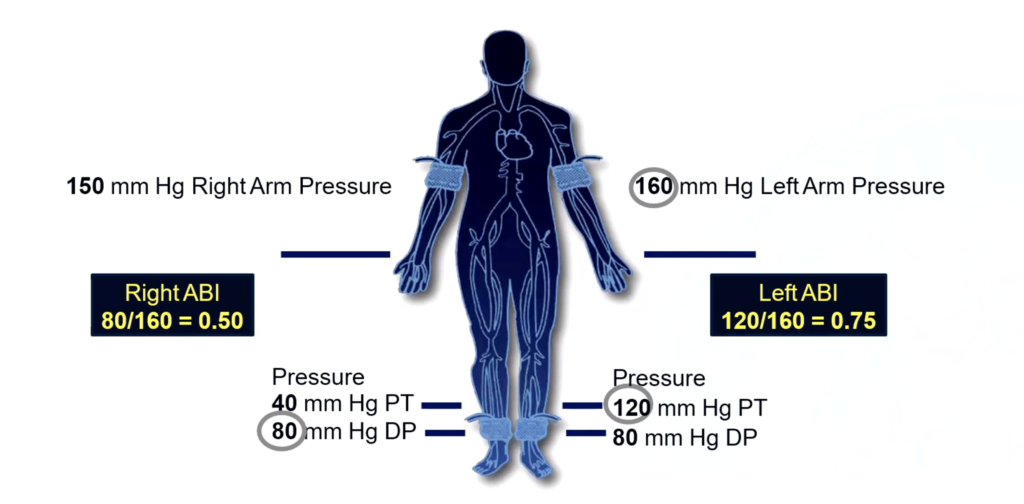
Ankle Brachial Index (ABI)
| ABI | Result |
|---|---|
| >1.4 | Non-compressible |
| 1-1.4 | Normal |
| 0.91-0.99 | Borderline abnormal |
| ≤0.9 | Abnormal |
** If >1.4: perform toe-brachial index. 20-30% increase is normal. >20 mmHg drop is abnormal
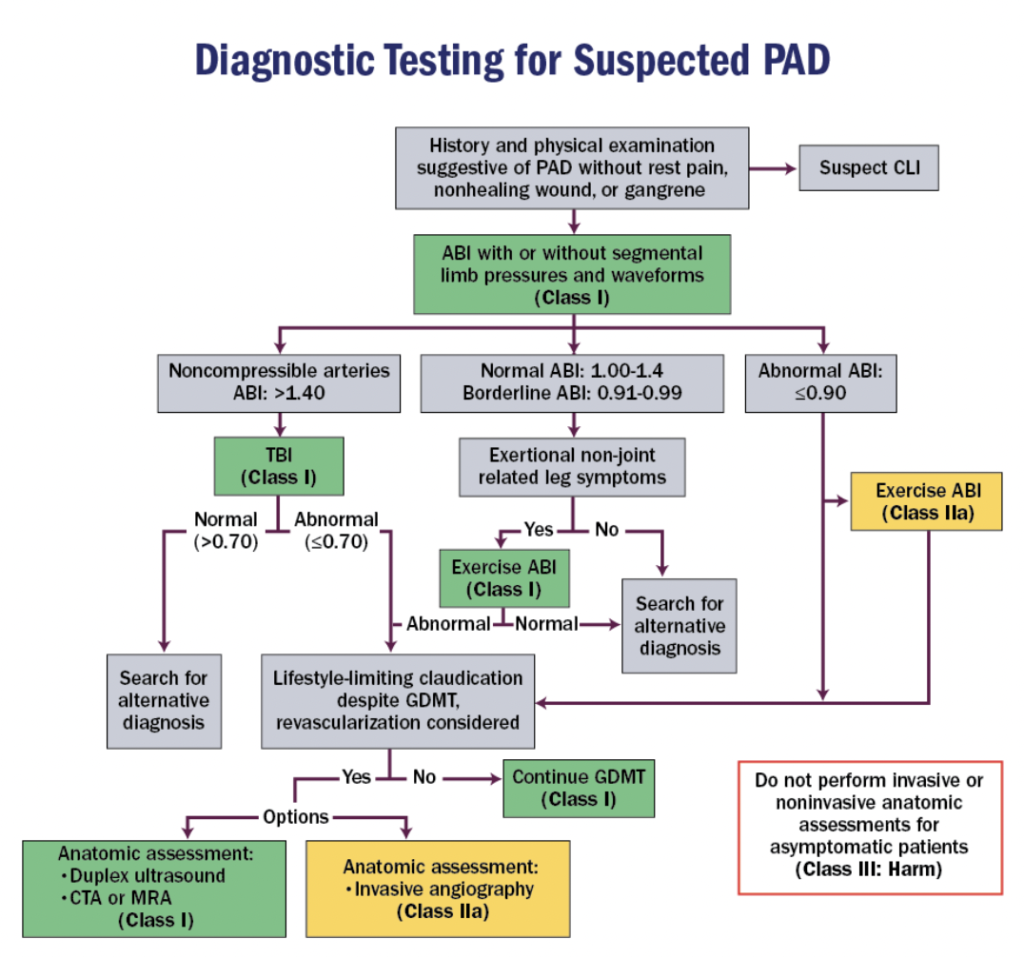
Screening for PAD
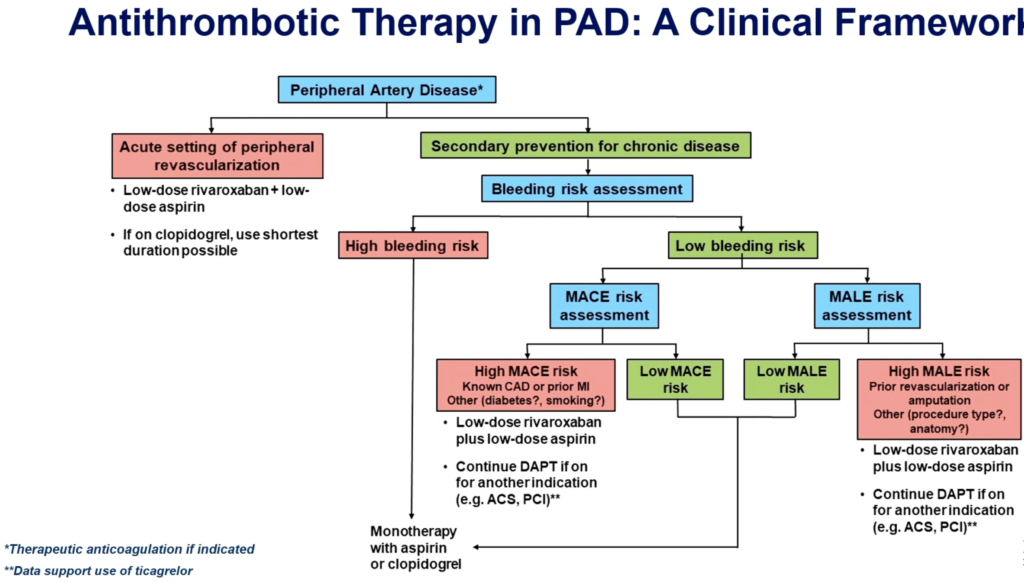
Treatment of PAD
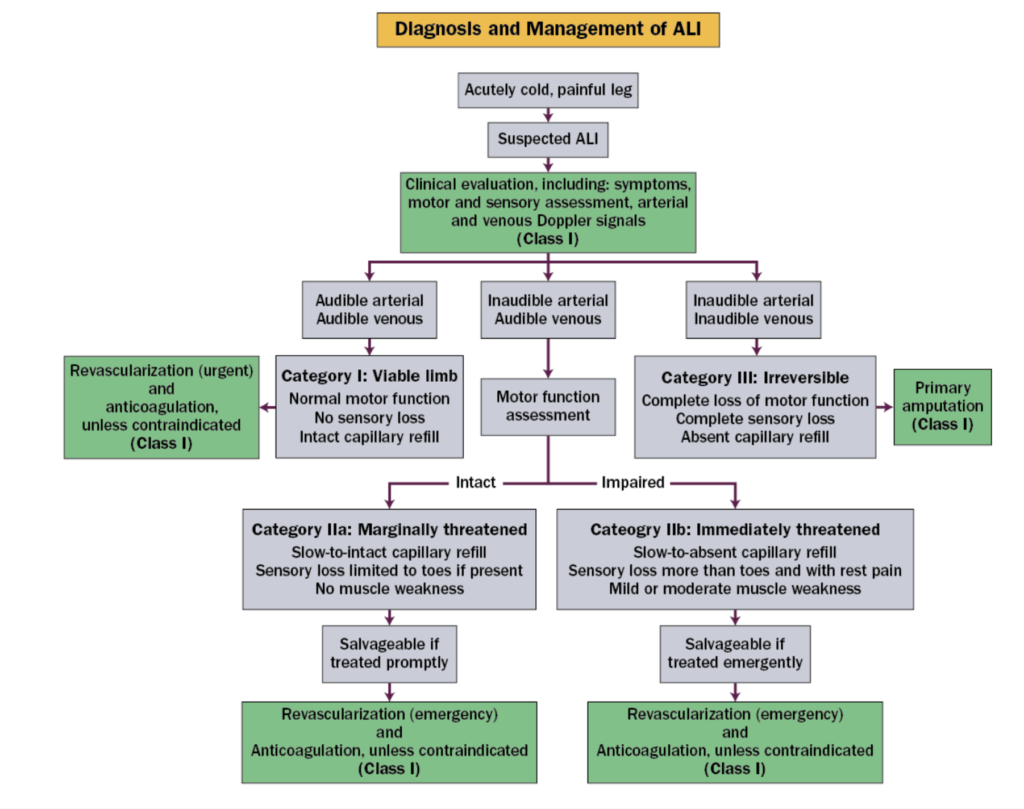
Acute Limb Ischemia (ALI)
Medium and Large Vessel Vasculitis
| Classification | Diagnosis | Etiology | Manifestations | Treatment |
|---|---|---|---|---|
| Large-vessel vasculitis | Takatasu arteritis | Age <50, > women, Asain, B-sypmtoms, ±erythema nodosum) | – 70% aortic lesions – Vascular inflammation ➡️ stenosis (long and tapering i.e. rat-tailing) ±aneurysm – Arm/leg claudication, mesenteric ischemia, stroke, renovascular HTN – Diastolic murmur, bruit, absent pulses | Steroids, IL-6i, TNFai |
| Large-vessel vasculitis | Giant cell arteritis | Age >50, >women, caucasian | – HA, jaw claudication, visual disturbances, stroke – ±Polymyalgia rheumatica (40-60%): stiffness, proximal muscle pain (RF, anti-CCP antibodies) – Subclavian, axillary stenosis/aneurysm, carotid/vertebral involvement | Steroids Tocilizumab |
| Medium-vessel vasculitis | Polyarteritis nodosa | Men, ~age 50, rare, associated with HBV infection Diagnosed clinically | B-symptoms, neurologic complaints (peripheral neuropathy), renal involvement, GI involvement, orchitis, cardiomyopathy, pericarditis, coronary involvement | Steroids ±Cyclophosphamide or azathioprine Antivirals if associated with active HBV infection |
| Medium-vessel vasculitis | Kawasaki disease | <5yo, Asain children (>Japanese), | 5 days fever, BL conjunctivitis, mucositis, rash, erythma, or desquamation of hands/feet, cervical lymphadenopathy | Untreated: ~25% develop coronary aneurysms Acute: IVIG ± aspirin. Sometimes steroids ±Anticoagulation if large aneurysms |
| Variable vessel vasculitis | Behçet’s disease | |||
| Variable vessel vasculitis | Cogan syndrome | |||
| Single-organ vasculitis | Isolated aortitis | |||
| Vasculitis associated with probable etiology | Infectious aortitis: syphillis, mycobaterial aortitis, suppurative/mycotic infectious aortitis Rheumatologic disease: IgG4-related disease, antineutrophil cytoplasmic antibody-associated vasculitis (ANCA), spondyloarthritis, Erdeim-Chester disease, relapsing polychondritis, sarcoidosis |