I know him as Joey from Brooklyn and had the pleasure to rotate with him before he was Dr. Seldin. Here’s what he had to say about his journey to landing a Physical Management & Rehabilitation (PM&R) residency.
Tell us a little bit about yourself. Who are you professionally? Who are you outside of the hospital? What was your path to medicine?
The best way to tell about myself is to start from where my family is from. My father is from Brooklyn and my Mother is from Queens. I grew up on Long Island and my wife is from the Bronx. And its not hard to tell when you talk to me, my accent says it all.
I went to college to the University of Buffalo and received a BS in Psychology. During this time I became very interested in Fitness and Nutrition, performed in Body Building Shows, and learned from one of the greatest Trainers in Buffalo John Schweikhard. This love for fitness and nutrition pushed me in the direction of perusing a masters degree in nutrition from Columbia University. While earning my Master’s I lived in Washington Heights and would spend my free time on the Upper West Side (UWS). One Friday in June of 2008 I was in a Bar on the UWS of Manhattan at a place called Burbon St. I was there early and she walked in, I looked at her and said “yo legs come over here” and we hit it off. At the end of the Summer, July 28, 2008 I was in a bad accident and lost my right eye. This was hard time for me. I finished my masters thesis a few months later. 90% of the people I studied with at Columbia went right into medical school all over the country.
I lost my flow, this was the first time in my life that I wasn’t in school anymore and didn’t have a job and didn’t know what to do. After a year and a half, when I had more confidence after loosing my sight and multiple surgeries, I fell back on my fitness and nutrition knowledge and decided to professionally train people. At the same time my little brother starting to box and I put a lot of effort into helping him train. I would make his meals and slept on his couch in return. Then I came to a point when I realized I needed to really go for what I wanted my whole life which was a to become a doctor. At this time I was professionally training several doctors and one of them who was a cardiologist said, ‘if you want it then go for it’. I took the MCAT and honestly very did poorly. So I took it again, and again and again. Finally I was at a party and this kid who was shadowing at one of my client’s offices was like, ‘I’m going to Ross’. I didn’t know anything about this school and said to myself it is worth a try.
Outside the hospital I am a family man, I had my son two weeks before the start of my 3rd year of medical school. It was hard to give time from my family and study but I pushed through. I had my 2nd child 6 weeks ago. She was due the day before we started residency but she arrived early. It was perfect timing because it gave me a chance to get to know her.
What specialties did you apply to? How did you come to choose them?
Before I started medical school, I came to know this field called PM&R, Physical Medicine and Rehabilitation. While I was training clients I came to build a lot of great relationships. One of them worked at North Shore LIJ hospital system and he helped me volunteer at their hospital in the PM&R division. I didn’t know it at the time but this small step may have gotten me the career I have today.
So I knew in my head before I started medical school that this may be the field for me. What most people don’t know is, I kept an open mind during my 3rd year of medical school and really enjoyed all of my rotations. The closest thing to PM&R for me was emergency medicine. I also met the best attending physician there who really inspired me and peaked my interested in that field too.
So I applied to both PM&R and EM.
So going into PM&R means you have to do a transition year. Did different programs have different requirements for that transition year?
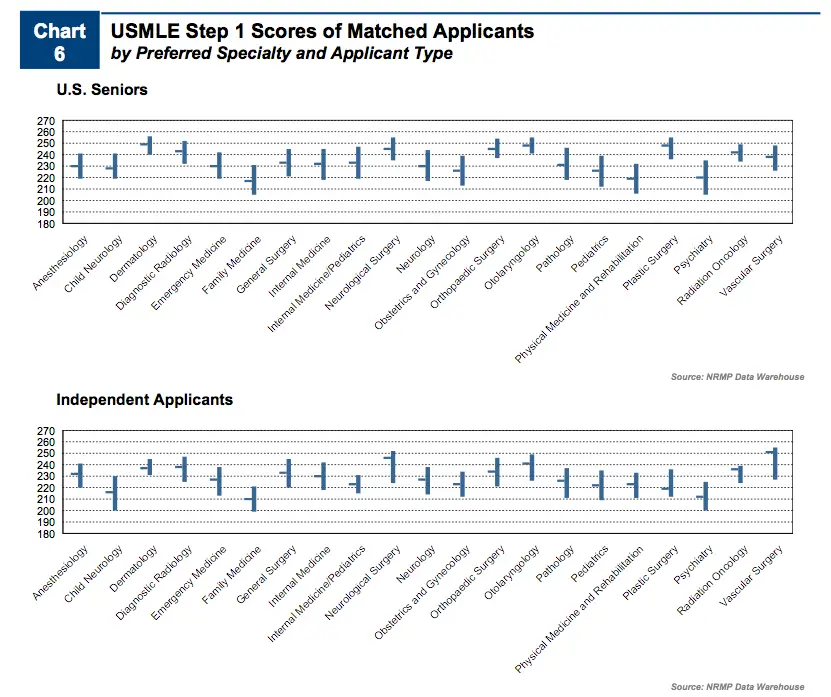
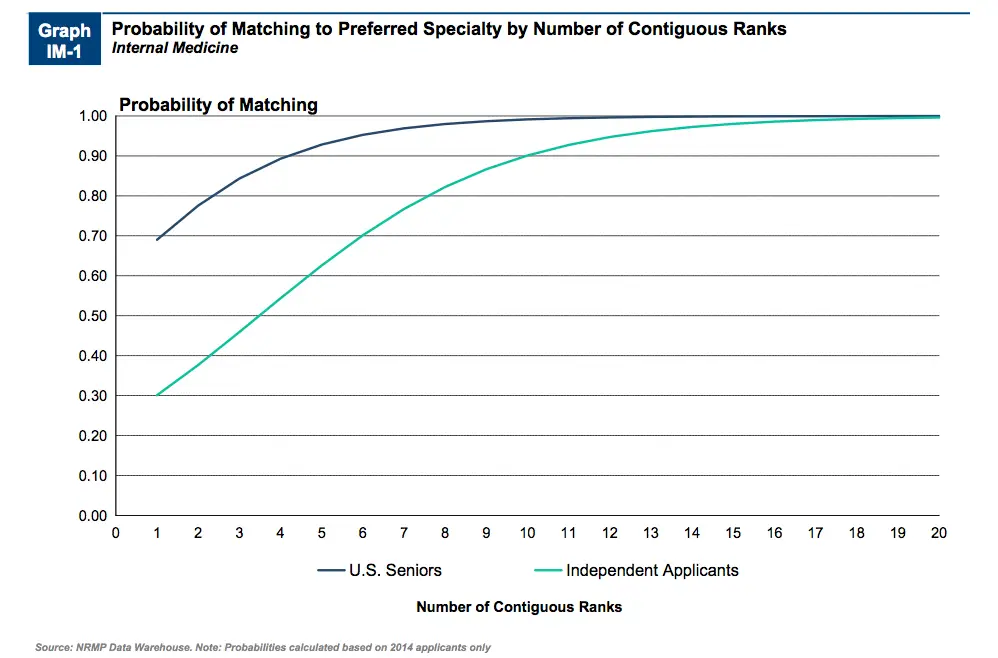
Most programs require you to complete a preliminary year in either internal medicine, family medicine, surgery, or a transitional year (this is like 5th year medical school- you rotate in surgery, OB/GYN, medicine, the ICU, EM, and some electives). Some programs have a categorical position, meaning you do your first year in that program as a medicine resident. Medicine is the most relevant in my opinion. The thing I didn’t know was that internal medicine preliminary spots are very hard to get. See, the ophthalmology, dermatology, radiology, and anesthesia guys and gals are going for IM prelim spots as well. So they’ve got the top step scores and they are US students. Where I am just in the top of the scores applying as an international medical graduate.
What was it like applying and interviewing for both of them?
I truly enjoyed the interview process and anyone who knows me also knows I am a talker. And when it comes to interviews, I thought to myself this is probably the only time I can get away with talking about myself all day. Another thing about applying to specialty fields is you don’t get interviews until October and until late December. It was mid October and I had like 4 interviews. My buddy applying to IM had like 20 by the end of September. Then all of a sudden I was bombarded with them.
How many programs did you end up applying to? What was your reasoning for that number of programs? How many interviews did you receive for each respectively?
I applied to 129 programs but I didn’t break the bank like other people I know. It ended up costing about $1,600. I applied to 10 transitional, 39 PM&R, 55 EM, and 25 IM programs. I got 10 PM&R, 10 IM Prelim, 6 EM, 1 TY interview for a total of 27 interviews. Of these interviews, 6 of these interviews I got by bugging programs to interview me and one of them is where I matched.
How did you end of ranking your programs?
My ranking was not an easy task. I went on a lot of interviews and honestly there a few things to consider for you rank. Some people rank based on location, academics, specialty, and other things. For me the most important was location. Staying in NY and being close to both my wife’s family and my family meant a lot.
What was the most challenging aspect of applying to PM&R?
There are not a lot of programs and in many programs are only 2-4 spots per year. I think there is only like 116 spots in the whole northeast.
For EM the IMG is non-existant these days. The programs are big into US students. There was lots of spots, lots of programs but I got only a few interviews.
Any crazy stories from the interview trail?
So SUNY Downstate PM&R pre-interview social, was at a bar in the village. It was open bar with top-notch drinks. The kicker was that we had to drink a certain amount to get a discount. So the residents had us downing beers and shots. I drank 6 Chimays and Duvels and downed a glass of Jonny Walker Blue. Then I had the interview the next day…good thing it wasn’t until 12pm.
What do you think were your greatest strengths about your application?
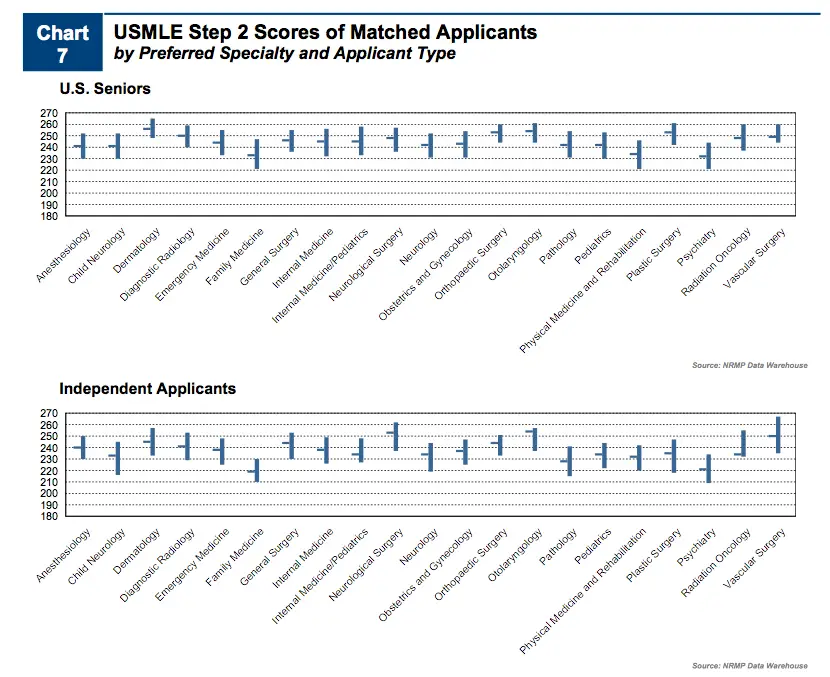
I applied locally. There are by far the most programs in NYC and having ties to an area can boost your ranking. I also scored very well. It is a special feeling when you go on an interview and pretty much know you probably have better scores then most of the people sitting next to you. If you go to Ross you know how hard it is to make it off that island and you know how hard you can work. I know I can work harder than anyone out there. I had a child right before my 3rd year of school and still was able to go up 17 points on step 2.
In contrast, what were your greatest weaknesses about your application?
The medical school I attended I would say was the greatest weakness. But is only the limiting factor for getting interviews. 80% for sure if you get an interview, they really want you otherwise they wouldn’t interview you.
My first interview was at Stony Brook PM&R, the director said, hey you go to Ross, great school. I laughed hard in my mind. Turns out that a resident many years ago at Stony Brook was a super star. On the flip side, there are hurdles with advanced match. See you can score a PM&R place on match day but that is only years 2-4 for your residency. You still need to also match in prelim as well. Now I matched in both of course otherwise I wouldn’t be talking to you about it. But sometimes a programs ranks someone in PM&R and the person doesn’t secure a prelim spot, and can’t soap into a spot either. Pretty much just fucked.
How did you do on the USMLE’s? What were your step scores? Do you think your step scores negatively/positively affected the number of interviews your received?
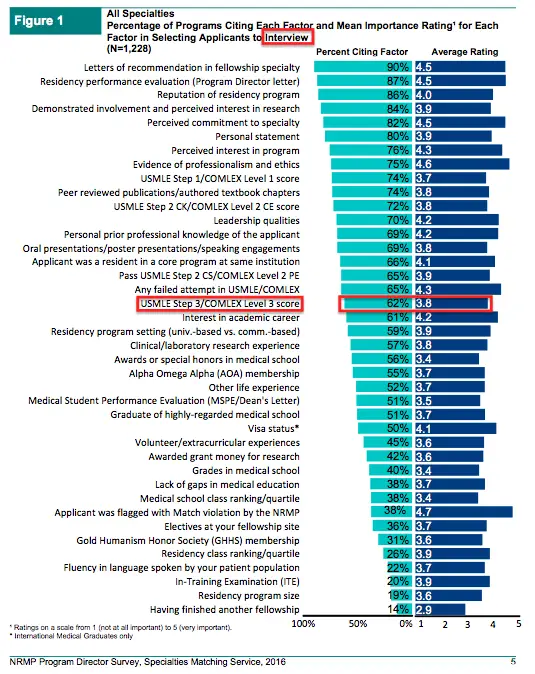
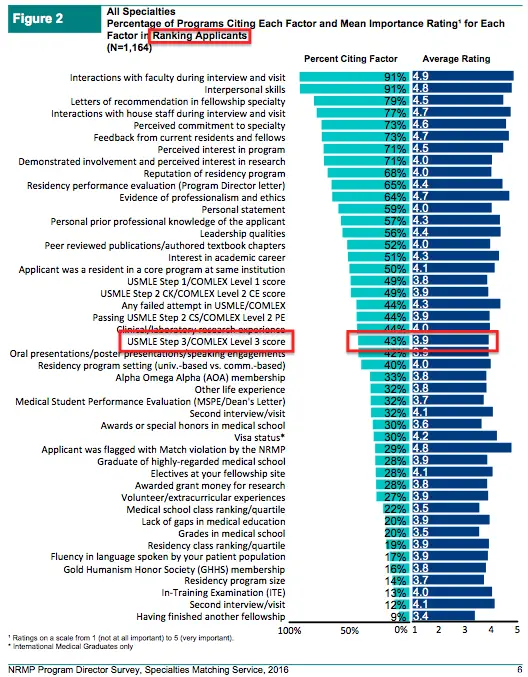
Step 1 242 and Step 2 257. They definitely helped me and I looked up the average scores on the ERAS stats list. No one scored as high as I did in 2014 in PM&R on Step 2. I know if my scores weren’t as good I would not have gotten close to the number of interviews I had.
What advice would you give to other Caribbean and/or American medical graduates who want to apply to PM&R?
Take every interview you can get. Also make sure you can rotate at a place that will let you go on your interviews during your rotation. On one of my electives I went on 4 interviews in one week and they didn’t give me any shit about it, which was great.
If you have shit scores, plan for back ups. Don’t be foolish. And if your scores suck, make sure you can relate to the field you are going for and kill it on the interview. I know one guy (and if he reads this will know who he is) has bad step one scores, but improved on step 2 but still under the average and landed a great residency. The reason is he related to the field and in the end of the day you only need one place to rank you (or two places if you’re going into PM&R…one prelim and one advanced spot). Even if it was your last rank, it’s better than nothing.
Take your test seriously. In June during my last 3rd year rotation I took a practice NBME and got a 220. I took another NBME one month later and got a 225. I finished 3rd year and had 4 uninterupted weeks to study. I took my 3rd NBME and got a 235. Took another 1 week later and got a 236. I wasn’t too happy at this point. But had got a lot down in the last 2 weeks of studying. 1 week before my exam, I took the USMLE World self-assessment got a 256 and was happy. 1 week later and got a 257. Holy shit was I happy.
Don’t worry about how many hours you will work as a resident in one field or anther. Before I started I didn’t know if I could really do this. But I did know I can push myself hard. Honestly I am up at 5 am every day, get to hospital 6-6:15am and finish about 5-6pm on a regular day. Not to mention short call and weekends. But I never feel like I can’t do it. You will do it. You’re so busy that the day flies by. You know your job is awesome when I go in on a Saturday at 6:30am and look at my clock and its 5pm and I need to get these last few notes done before sign-out. You can do it too I promise. I really can say that I love my job.
Thank you Joey for giving us a candid look at your application process. Be sure to subscribe so you don’t miss my second interview with an unmatched psych applicant.