Dermatology is one of the most competitive specialties in medicine. Today I sat down with Benny Wu who is a current dermatologyy resident at Broward Health Medical Center. He shared his journey to dermatology and some advice on how to match into derm.
Thanks for letting me pick your brain, Benny. Can you tell my readers a little bit about yourself?
It is an honor for me to share my path to Dermatology residency with your readers and followers. I am currently a PGY-2 Dermatology Resident at Broward Health Medical Center in sunny Fort Lauderdale, Florida. Before medical school, I was a figure skater for thirteen years – competed on the national and international level. In 2005, I chose to end my competitive skating career due to recurring injuries and realized it was ‘time’ to move forward with life by pursuing my second passion: medicine and science. Unfortunately, during college, I did not juggle my college coursework and figure skating very well. I had an embarrassingly low G.P.A. from the University of California, Irvine and did terribly on my MCAT. The next pivotal moment that had a direct impact on my medical career came in 2007. A medical school formerly known as the University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine, now called Rowan University School of Osteopathic Medicine (RowanSOM), offered a Master’s in Biomedical Sciences degree for students who performed poorly during college but remained interested in attending medical school. RowanSOM advised me that my chances of being accepted into their medical school would be greatly increased if I performed exceptionally well in the Master’s program and if I improved my MCAT score. I performed extremely well in the Master’s program and brought my MCAT score way up (I distinctly remembered in 2005, my Physical Science score was 5/15, but in 2008 my Physical Science score went up to 10/15). Luckily, I was accepted into RowanSOM’s D.O. program in 2008. During the Master’s program and pre-clinical years I fell in love with immunology and became invested in how the body worked from the cellular and molecular level. Because of my fascination with immunology and medical research RowanSOM invited me to complete the D.O./Ph.D. combined program in 2011. Outside of medicine, I enjoy staying physically active (running and cycling) and cooking. One of my therapeutic outlets is cooking with fresh ingredients accompanied by a glass (or several glasses) of wine!
What motivated you to pursue dermatology?
Answering the following two questions can best explain my motivation for pursuing Dermatology
(1) What interests me in Dermatology – Dermatology requires a STRONG background and fund of knowledge in Internal Medicine and its subspecialties (Infectious Disease, Rheumatology, Nephrology, Pulmonology). Response to treatment is readily appreciated and is not heavily dependent on laboratory findings. One example I share with medical students is this – imagine being able to make a clinical diagnosis and assess response to treatment independent of lab findings – of course, more often than not, a confirmatory diagnosis will require a skin biopsy (side note: there are lots of procedures in Dermatology, too!). On the other hand, as much as we would like to refute this way of thinking, the importance of outward appearance in our society, and how it impacts one’s sense of self-worth, cannot be ignored or disregarded – just ask any severe nodulocystic acne patient how he feels after a full course of Accutane – it really is life-changing!
(2) What problems do I think Dermatology faces – I emphasize the difficulties because issues in any specialty can serve as motivating factors for medical students and young attendings. In Dermatology, the pathophysiology of many skin conditions remain unclear or unknown – there is a lot of opportunities for both basic science and clinical research in Dermatology. However, the more pressing concern is the dwindling interest in complex medical Dermatology – this may be due to decreased reimbursements from insurance carriers – but I see this unique problem as an opportunity for Dermatologists-in-training to start new Dermatology fellowship programs, such as Dermatology Hospitalists. For example, severe pemphigus patients admitted for rituximab infusion – this is classically a Dermatology-driven problem that can be managed by the primary Dermatology service.
Something that impressed me about you is that how persistent you were in pursuing your desired specialty. You didn’t match into dermatology…twice. But you persisted and landed a residency position in your dream job. What did the experiences of not matching into dermatology teach you?
Not matching into Dermatology taught me the importance of focusing on my modifiable weaknesses.
After failing to match again during my intern year at Drexel, I had to ask myself two questions: (i) is Dermatology the only specialty for me? (ii) if so, what can I do to maximize my chances the third time around?
Facts are facts. I am a D.O. with average USMLE scores for Dermatology (these are not modifiable). However, my lack of publication and research experience in Dermatology was modifiable. Thus, I made a promise to myself that I would give myself one last chance – reapply to Dermatology – but this time as a Northwestern Dermatology Clinical Research Fellow.
Also, I learned how much ‘grit’ I have. Dr. Angela Duckworth’s book, “Grit: the power of passion and perseverance” discussed the importance of being ‘gritty’ especially when dealing with failures or disappointments. If you have not read this book, I urge every one of your followers to read it, especially before the interview season begins – I believe in the two equations outlined by Dr. Duckworth: talent x effort = skill; skill x effort = achievement; TALENT counts ONCE while EFFORT counts TWICE.
Why do you think you didn’t match multiple times?
I failed to match numerous times because of the following reasons:
- Did not initially consider D.O. Dermatology programs
- Did not apply broadly (limited myself geographically).
- My degree, D.O. – Dermatology is a competitive specialty even for U.S. M.D. graduates.
- Average to below-average USMLE Step 1 score (238) for matched applicants – as a D.O., a spectacular Step 1 score (>250) would have helped – but not a guarantee by any means.
- CV did not differ much between the first and second time applying.
What did you do differently the second time to improve your chances of matching? Why do you think you failed to match a second time?
I did not do anything differently the second time around – as you know, we were co-interns at the time and had limited time to add significant publications or research experiences to my CV. The only addition to my CV in the 2017 cycle was one publication – a review article on drug-induced pyoderma gangrenosum.
So you finished your required preliminary year in internal medicine and you are offered the opportunity to stay and complete a categorical three-year residency in internal medicine. Why didn’t you stay?
Do you want a fluffy answer or the real answer? ☺ I did not stay because Dermatology remained one of the few medical specialties that I could see myself doing long-term. However, I loved infectious disease as well. Like I said before, there was one modifiable ‘weakness’ in my application – Dermatology research experience. Near the end of intern year, I was offered a Dermatology Clinical Research Fellow position at Northwestern University, Feinberg School of Medicine. Privately, I told myself that if I did not match the third time around, I would complete Categorical-Medicine residency and possibly pursue Infectious Disease.
What did you do professionally after your preliminary year to improve your application while you re-applied for the third time?
Right after the Medicine-Preliminary year, I moved to Chicago and completed a Dermatology Clinical Research Fellowship at Northwestern University. Simultaneously, I entered the 2018 ERAS and NRMP and applied with new recommendation letter writers (2 from Northwestern Dermatology Faculty, 1 from University of Pennsylvania Dermatology Faculty, 1 from Drexel/Hahnemann University Hospital Medicine Residency PD) and 1 new publication (ichthyosis, X-linked) with the Northwestern Dermatology Chair, Dr. Amy Paller (https://www.ncbi.nlm.nih.gov/pubmed/28846233).
Thankfully you matched. What do you think you would have done if you didn’t match for a third time?
If I did not match, after three attempts, I would have done the following in sequential order:
- Try to secure an unfilled position through the SOAP.
- Apply to the few programs that secured extra funding for more spots or received ACGME-approval to increase program size after the NRMP Match quota deadline. Because Dermatology is a relatively small community, one advantage of doing a research fellowship at a major academic institution, such as Northwestern, is that PDs will advertise open positions on a listserv available to only Association of Professors of Dermatology Members (Dermatology PDs). Northwestern forwarded open positions to their research fellows since 2 out of 5 research fellows did not match.
- If number 1 and 2 don’t work in my favor, then I would seek out available PGY-2 Medicine Categorical positions, with the hope of specializing in Infectious Disease later down the road.
How many dermatology programs did you apply to each year? How many did you rank?
– In 2016, I applied to ~50 Dermatology Programs and 18 Medicine-Preliminary Programs. Ranked 5 Dermatology Programs (NRMP).
– In 2017, I applied to ~90 Dermatology Programs (including both Advanced ‘A’ and Physician-only ‘R’ positions). Ranked 2 Dermatology Programs (NRMP).
– In 2018, I applied to 95 Dermatology Programs (15 AOA-accredited “D.O.” programs and 80 Dermatology Programs – including both ‘A’ and ‘R’ positions). Ranked 2 AOA-accredited Dermatology Programs (NMS Match). Ranked 6 Dermatology Programs (NRMP)
What advice do you have for medical students who want to pursue dermatology?
– Read, read, and read more: highly recommend Lookingbill and Marks Dermatology textbook – this is a basic Dermatology textbook – very user-friendly.
– Approach to reading primary research articles: learn how to interpret and formulate questions as you read research articles – (i) is the study design robust – assess strengths and weaknesses (ii) any bias (iii) does it directly address the hypothesis – keep in mind that negative papers can still be valuable (iv) author financial relationship disclosure – is there a conflict of interest? Learning these skills early on will help you tremendously at audition rotations – this will quickly set you apart from other applicants – always remain inquisitive.
– Align yourself with a Dermatology mentor as soon as possible: if your school does not have a home Dermatology Department then search for a local Dermatology Society (for example, Chicago Dermatological Society [CDS] and PhillyDerm in Philadelphia, PA).
– No need to submit to only Dermatology journals: if you see a compelling case in your non-Dermatology clerkships that is Dermatology-relevant (for example, VZV reactivation in an immunocompromised patient) submit the case as a Continuing Medical Education (CME) quiz to a Family Medicine or Internal Medicine journal.
– Ask yourself these question: “is Dermatology the only specialty I see myself doing?” Remember, Dermatology has significant overlap with Rheumatology, Infectious Disease, and Family Medicine/Primary Care. By not limiting your publications to Dermatology journals, should you decide to apply to Family Medicine or Internal Medicine down the road, it will appear less likely that you ‘settled’ for another specialty.
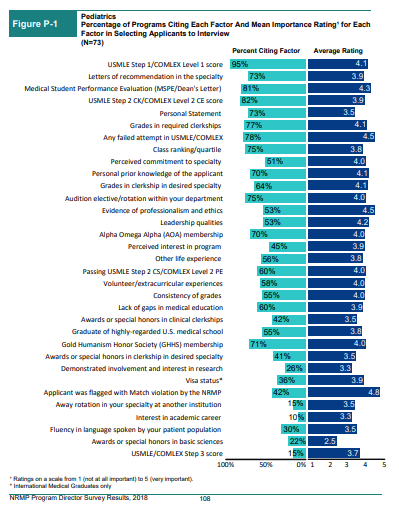
What are important aspects of a residency application for dermatology? Is it heavily research oriented?
– Research is critical (except for a few Dermatology programs, most are academically-driven and require residents to publish annually). Many of the applicants I met on the interview trail took a year off to do research. However, a dedicated research year is not critical – instead, focus on getting 2-3 FIRST author PMID (PubMed Indexed) publications by the time ERAS is ‘due’ (typically ~ September 15)
– First authorship holds much more weight – keep in mind papers can come in a variety of flavors: case-reports, case-series, CME quizzes, and review articles.
– By taking command of your publications, this will serve you well during the interview – you may be interviewing with a faculty member who is an ‘expert’ in the topic of your research or publication(s).
Any residency interview tips specific to dermatology that you wish someone told you before you hit the interview trail?
(i) Please do not discount the value and importance of PCs! I believe that Kaiser-Los Angeles Dermatology granted me an interview because I was professional and courteous when communicating with the PC.
(ii) Compile a list of programs that you would like to receive an interview – construct a personalized letter of interest to each program – outline the reasons why that program is attractive (besides being Dermatology!) – email the letter to the PC in late September so it can be added to your file for review.
(iii) Pay attention to your speaking volume and level of engagement during the pre-interview dinner and interview day – I lived by this saying ‘loose lips sink ships.’
(iv) If you are placed on the wait-list, email the PC and ask when the interview(s) are held? – Three weeks before the interview date(s), send the PC an email reminding him/her of your interest and provide application updates, if applicable.
(v) Avoid emailing or calling the PC with general questions about the program – study and thoroughly comb through the program websites.
(vi) Only reserve emails when you have SIGNIFICANT application updates – for example, I was asked to give an oral presentation at the 2018 American Academy of Dermatology (AAD) Annual Meeting [https://www.aad.org/scientificsessions/am2018/SessionDetails.aspx?id=11492] after I certified my ERAS – after updating my programs of interest, I received an interview invite from one program several hours later.
(vii) After the interview, prepare handwritten thank you cards for the PD and PC – note: in 2018, several programs explicitly stated NO thank you cards.
(viii) Prepare written templates for the following scenarios: (a) requesting letter of recommendations (b) accepting interview invites (because rarely do Dermatology applicants reject interview invitations) (c) letter of interest – tailored to specific programs (d) post-interview thank you card (e) top choice/you are my number one letter. I have templates (Dermatology-specific) for all these scenarios – please contact me directly if you wish to see my templates.
(ix) Avoid post-interview communication with the PD, PC, and residents – unless it is for SIGNIFICANT application updates – also, no harm in sending your number one a letter of intent several weeks before the rank list is due – note: in 2018, several programs explicitly said no post-interview communications.
Here are some facts for you and my followers. In 2016, based on NRMP match rate data, dermatology was the 5th most difficult specialty to match into behind only neurosurgery, orthopedic surgery, plastic surgery, and vascular surgery. Likewise in 2016, dermatology was among the six specialties with the highest average USMLE step 1 score for applicants who matched into their preferred specialty along with neurosurgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. That average USMLE step 1 score was 250. Although I believe that high board scores shouldn’t be the only important aspect of a medical student’s residency application, it is hard to argue with objective data in that if you want to match into a highly competitive residency like dermatology you need to ace your boards. What advice do you have for medical students who want to pursue dermatology but don’t have those ultra-competitive board scores?
I scored a 238 on my USMLE Step 1 (please keep in mind that I took my Step 1 in 2011 – the passing score changed several years later). Regardless, 238 is not a strong score for Dermatology. If you scored <240 on USMLE Step 1, focus on the modifiable aspects of your application – (i) research – aim for 3 to 4 first author publications (ii) mentorship – seek out mentors as soon as possible so you have time to develop a relationship with them – this will lead to STRONG letters of recommendation (iii) research year – consider a research year (between MS III/IV) – I highly recommend the Northwestern Dermatology Pre-Doctoral Fellowship (iv) I cannot stress this enough – if you want to pursue Dermatology, remain focused on the modifiable aspects of your CV!
How did you find and develop a relationship with a mentor in dermatology?
My Ph.D. was on neutrophil biology in sepsis. Naturally, I asked myself the question “which skin conditions are driven by neutrophil dysfunction?” I found out that several neutrophil-mediated skin diseases fall under the spectrum of diseases commonly known as ‘neutrophilic dermatoses (ND).” As a fourth-year medical student, I reached out to Drs. Misha Rosenbach and Robert Micheletti from the University of Pennsylvania Dermatology (they are both Dermatology Hospitalists and have research interests in ND) – I contacted them and expressed my interest in Dermatology and ‘expertise’ in neutrophil biology. At that time, they happened to be in the process of spearheading a retrospective chart review of patients admitted with Sweet’s syndrome! Long story short, I completed two months of research with them, and they became my mentors through this process. Although I was not a University of Pennsylvania medical student, Dr. Micheletti supported my Dermatology Residency Application all three times – Dr. Micheletti emailed me on Match Monday, one hour after NRMP released the much anticipated “Did I Match?” email, and asked how I am doing and if I matched. Mentors do not have to be from your home institution. The mentor-mentee relationship takes work – take these relationships seriously but also show your ‘humanistic side’ or ‘brand of personality’ when appropriate. Remember, there are MANY ways to find and develop a relationship with a mentor – this is just one example of how I did it.
What is the biggest misconception about the field of dermatology?
The biggest misconception about Dermatology is that it is an ‘isolated’ specialty – like I mentioned before, Dermatology overlaps with many, if not all, of the Internal Medicine subspecialties – think: systemic lupus erythematosus (Rheumatology), HIV-associated dermatoses (Infectious Disease), systemic sclerosis (Rheumatology, Nephrology, Gastrointestinal, Pulmonology). There is significant overlap between all of the previously mentioned specialties – we see more multidisciplinary clinics, such as Rheumatology-Dermatology, for connective tissue disease patients with skin manifestations. Again, you do not need to limit your manuscript submissions to Dermatology journals – many internal diseases present on the skin – for instance, a CME quiz or review paper on atypical presentations of sarcoidosis can be submitted to a Pulmonology journal.
What are the strangest, most bizarre, or most unique questions you’ve been asked after people find out that you’re going into dermatology?
What people commonly say when they find out I am a Dermatology Resident is “oh, that is why you have such nice skin.” The most common question is “what should I do about X, Y, and Z (insert common COSMETIC complaints here) – because of this, I tell new people I meet that I am a Medicine Resident ☺. Also, my phone will occasionally receive pictures of rashes and bumps from my friends – I usually respond with “not interested” haha, just kidding! All jokes aside, I enjoy the question “why Dermatology?” – this question reminds me of the reasons why I chose to pursue Dermatology – and I take this opportunity to educate the public that Dermatologists are not merely ‘pimple-poppers, cyst-removers, and soft tissue injectors.’
Okay, so now the question that I’m sure you must be asked non-stop: what’s your skincare regimen?
Well, I do have pretty fabulous skin… ☺ haha. Disclaimer: ‘healthy’ skin is heavily driven by his/her genetic makeup – but evidence-based medicine suggests that sun protection and intact skin barrier are critical for optimal skin health. And of course you should not use this as medical advice. If you have skin questions or concerns you should always seek out an expert consultation with a dermatologist. This is my skin care routine:
Morning
In the shower: limit shower time to <10 min and use lukewarm, NOT HOT, water.
(a) Panoxyl 10% benzoyl peroxide (BPO) face and body wash – apply wash to my face only – prevents acne breakouts – has antibacterial and anti-inflammatory properties (BPO will whiten colored clothing so make sure you thoroughly rinse off the BPO, especially if you use colored towels).
(b) Cetaphil Gentle Cleansing Bar Soap.
Post-shower
If you are prone to eczema or dry skin – use towel to damp dry – followed by emollient (cream-based, not lotion) application – emollient will ‘lock-in’ moisture.
– Cetaphil Men’s Daily Facial Moisturizer SPF 15 – quick word about SPF – unless you have a genetic skin disease (i.e. Gorlin’s syndrome) – no need for SPF>30 – SPF and percentage of UV blocked employs a base-10 logarithmic scale – this means that an SPF of 10 blocks out 90% of UV, SPF 15 blocks out 93.3% of UV and so forth – the percentage of UV blockage basically levels off above SPF 30 – save your money and spend it on an excellent emollient, instead – see below.
– Cetaphil or CeraVe Moisturizing Cream (from tub NOT pump or squeeze bottle) – I use this to prevent moisture loss and to maintain an intact skin barrier – this is especially important for long hours in the hospital (definitely experienced this as a Preliminary-Medicine intern) – apply liberally to arms and legs.
Evening
Same as morning routine (BPO face wash) with the addition of topical retinoids – retinoids such as adapalene 0.1 or 0.3%. Retinoids are indicated for acne and pre-cancerous skin lesions, but they have also demonstrated repeatedly in several controlled studies to improve fine wrinkling, increase dermal collagen synthesis, and lighten uneven pigmentation – because of these reasons, I use adapalene 0.3% nightly – if your insurance does not cover retinoids (tretinoin, adapalene) it can be purchased over-the-counter under the brand name Differin (adapalene).
Things to avoid
Alcohol-based products (dries skin) and anything scented.

Benny Wu was born in Taipei, Taiwan and immigrated to the United States (Cupertino, California) when he was 10 years-old. Before medical school, he was a figure skater for thirteen years – competing on the national and international level. He graduated from the University of California at Irvine (Irvine, California) the same year he decided to end his competitive skating career. Before attending Rowan University School of Osteopathic Medicine, Bennybecame interested in medical research while he earned a Master’s of Biomedical Sciences from the University of Medicine and Dentistry of New Jersey. This led him to enroll in the combined D.O./Ph.D. program at Rowan University in 2009. Upon graduation from Rowan University in 2016, Bennycompleted an intense but rewarding Medicine-Preliminary internship year at Drexel/Hahnemann University Hospital in the ‘City of Brotherly Love’ (Philadelphia, PA). After his internship year, Benny fully immersed him in Dermatology clinical research by completing a Dermatology Clinical Research Fellowship at Northwestern University, Feinberg School of Medicine. Besides immunodermatology and translational research, he is passionate about mentoring medical students serious about pursuing Dermatology. Outside of Dermatology, Benny enjoys cycling, completing workouts that incorporate stability, endurance, strength, and athletic power, cooking, baking, and traveling. His next dream vacation spot is South Africa (cage dive with Great Whites). To learn more about Benny including his winding path to a dermatology residency you can follow him on Instagram at dermination_sk8r.
Interested in other specialty specific resident interviews? Check out these resident interviews and subscribe so you don’t miss out on the next blog post!
https://mykittykatz.com/what-happens-when-you-dont-match-into-residency-twice/
Like this:
Like Loading...