I just started a new YouTube channel! My first three videos are on Caribbean med schools, why I chose to pursue an internal medicine residency, and how to get a cardiology fellowship and become a cardiologist in the US. Watch them below and be sure to subscribe! The next videos coming out will be patient centered about heart health!
How To Match Into Gastroenterology Fellowship
I’m excited to share my next interview. Keerthi Shah was a senior resident at my residency program and is now a first year gastroenterology fellow at Hahnemann University Hospital/Drexel University College of Medicine.
Thanks for letting me pick your brain Keerthi. Can you tell my followers a little bit about yourself?
I would love to! I’m a PGY-4 or a first year Gastroenterology (GI) Fellow at Drexel University College of Medicine.
I grew up in Georgia most of my life. I went to Georgia Technology for undergrad and then Philadelphia College of Osteopathic Medicine for medical school (the GA campus). When I’m not practicing medicine I love to dance and travel. I’ve been learning, teaching and performing kuchipudi, an indian artform, since I was 7!
I’ll start off with another softball question and take you back to your residency days. Why did you go into medicine?
I was always pretty sure that I wanted to do medicine and then specialize. Combining patient histories with objective data to figure out the diagnosis was like a puzzle. I liked that kind of challenge. In addition, having such a broad knowledge base prepares you for any future fellowship.
Did you always know that you wanted to go into GI?
No! I was between nephrology and gastroenterology when I started residency. These two fields are worlds apart!
The biggest reason I found my way to GI is the procedures. There is such a satisfying feeling about working with your hands and learning a new technical skill. Even during my time in medicine, I enjoyed placing central lines and performing paracentesis. I knew the learning curve would be very steep, but I was ready for that challenge!
To be extra sure of this path I spent months exploring gastroenterology and hepatology, both inpatient and outpatient. All this time just made me more sure and excited.
GI fellowship is three years. What are the subspecialties in GI and how long are they?
There are 5 main subspecialities in GI: (1) motility and functional GI disease, (2) Inflammatory Bowel Disease, (3) advanced endoscopy, (4) nutrition/obesity and (5) hepatology/transplant hepatology. You can choose to do an extra year or you can attend symposia and workshops to build those skills. You essentially don’t have to do the extra year to be able to practice most of those subspecialities. The only exception is advanced endoscopy and trnsplant hepatology which is 2 years and 1 year respectively.
Do you think you will stay as a general gastroenterologist or do you plan on pursuing a subspecialty?
I’m fortunate to be at a program that exposes fellows to subspecialities. Honestly, I’m just enjoying learning about every area of GI. Motility, nutrition, and IBD are areas of focus that I’ve particularly enjoyed. For right now though, I plan to stay general gastroenterology.
I remember you telling me about a pretty alarming turn of events during interview season that almost left you without a fellowship. What happened and what lesson should fellowship applicants take away from it?
I’ll start out saying I’m an osteopathic physician. When I was applying, I applied to both MD and DO programs. Some of the DO programs are still outside of the match process. I interviewed and got accepted at one program. After a lot of thought, I accepted the position and cancelled the rest of my interviews. A couple days before the match, the program contacted me saying they could no longer give me the position because of internal issues. I scrambled to get interviews back. Luckily everything worked out and I matched at my home program. Needless to say, this was a stressful couple of days! The moral of the story is to not cancel anything till the contract is signed.
Gastroenterology is one of the most competitive internal medicine fellowships. What are the most important aspects of a GI fellowship application?
Great letters of recommendation, which stems from good mentorship, are the most important part of your fellowship application. Take the time to get to know the GI attendings at your home program. Work in the inpatient and outpatient clinics.. Get letters from these physicians! Their names are known in the GI community and getting a great recommendation will go a long way.
Research is a must for competitive fellowships like gastroenterology; however quality is valued over quantity. Programs like to see that you took a project to completion from conception to poster/oral presentations and eventually to publication.
Lastly, work hard! People will notice your hustle and that will make your LOR’s even better.
What research did you do during residency?
My first project was assessing quality of life (QOL) in transplant recipients and the use of group experiences to improve QOL. I was fortunate to be able to present this at an international conference and very recently published in Pediatric Transplantation Journal.
I did mostly hepatology research because my first mentor at Drexel was Dr. Santiago Munoz. The two notable projects were addressing etiology and prevention of hyponatremia in cirrhosis at an inner city hospital and expanding inclusion criteria for Obeticholic Acid in Primary Biliary Cirrhosis. Both projects were presented at GI conferences.
From there I expanded to gastroenterology. I worked with our Motility focused attending on evaluating Dysynergic Defecation with 3D High Resolution Anorectal Manometry.
Did you do any quality improvement projects?
I did one quality improvement project analyzing and improving night float and nursing communication using cell phones and text paging. The current pager system is such an archaic interface for communication. Our hospital is now transitioning to a phone based night float system.
What general advice do you have for prospective residents who want to pursue gastroenterology?
Spend time getting to know the GI program at your hospital. Work with them inpatient and outpatient. Do research with them.
The hardest part of fellowship is the volume of consults and learning a new technical skill. Hard work and a good attitude will go a long way.
You recently started a blog. Tell me about it. What’s your vision for your blog?
I recently started this blog initially to answer questions from my friends and family. I wanted to be able to provide them with answers that were based on up to date literature.
Our interactions with patients in the clinic are so brief. In 15 minutes, we are expected to take a history, diagnose, and treat. This leaves patients’ with a lot of questions and they seek their answers on social media. I wanted to be a part of the social media dialogue. I also wanted this to be my way of supplementing abbreviated clinic time to explain gastroenterology topics to patients in an effective way.
Where can my followers find you on Instagram? What can the expect to see?
In a nutshell, my Instagram is a combination of 3 things: GI, travel and friends/family. When it comes to gastroenterology I hope to perpetuate evidence based information as well as tips and tricks for aspiring GI fellows.
What’s the weirdest question people ask you after they find out you’re a GI fellow?
Honestly nothing weird! People ask me a lot of questions regarding their bowel movements. I think the strangest part of being a fellow is the number of pictures of stool I have on my phone.
How much poop is too much poop?
Well, everyone’s “normal” is different! Too much poop for you might be someone’s normal! The number of times you go isn’t as important as the consistency of your bowel movements. If you’re having 3 or more loose/watery Bristol 5-6 bowel movements, we need to talk!
Why do you get the day after drinking diarrhea?
Acute alcohol consumption inhibits absorption of nutrients and fluids. this stimulates secretion of water and electrolytes. effect of alcohol on CNS increases colonic motility and transit time. This prevents absorption of water in the large intestine. If you are drinking sugary mixed drinks, you might be drinking sugar substitutes, which causes osmotic diarrhea.
A patient recently asked me about constipation. What are some common home remedies patients can try?
Constipation affects so many people and results in many hospital admissions. Some things people can do at home include exercise, fiber supplementation, answer nature’s call, and improve your stooling posture. Osteopathic Manipulative Medicine (OMM) can also be helpful. Check out my blog post for more details!
Thank you so much for sharing some insight into the world of gastroenterology Keerthi. As always be sure to subscribe below so you don’t miss out on the next post!
How To Match Into a Hematology & Oncology Fellowship
Joel Alcid is a third year internal medicine resident finishing up his final year of residency at Hahnemann University Hospital/Drexel University College of Medicine. Next year he will be starting his fellowship training in hematology and oncology. I sat down with him to learn more about how he earned this monumental achievement and tips for medical students and residents who are interested in pursuing a heme/onc fellowship too
Thanks for letting me pick your brain Joel. Can you tell my followers a little bit about yourself?
Thank you for this opportunity. I am happy to share my thoughts and provide some guidance for those who are interested in pursuing a career in hematology/oncology. But first here are some fun facts about me
- I am Filipino-American
- Born and raised in North Jersey
- Attended the University of Hartford and majored in respiratory therapy (yes, I originally thought of pulmonary/critical care prior to med school)
- Attended the American University of Antigua for medical school
- I’m a huge boxing fan, my favorite boxer is of course…Manny Pacquiao
- I currently train at James Shuler’s Gym in West PhillyI recently got married in August of this year in Riviera Maya, Mexico
Did you always know you wanted to pursue hematology and oncology (heme/onc) fellowship? What about it attracted you?Yes. I knew since my third year of medical school that I wanted to pursue a career in hematology/oncology. I was always interested in the variety of pathology within the field, especially the cancer aspect. During my fourth year of medical school I was fortunate enough to do a one-on-one sub-internship rotation with an attending in his private practice. I had the chance to gain firsthand experience of what a career in heme/onc would be like. The diversity and complexity of the cases I was seeing on a daily basis attracted me to this specialty. From a patient with recurrent invasive ductal carcinoma who had developed metastasis to bone to a patient with a skin lesion that was diagnosed as mantle cell lymphoma.
Another aspect of the field that I developed immense respect towards during my rotation was the chance to support patients through their emotional struggles. Close patient contact and forming relationships with the patients is an important aspect of medicine in which I really enjoy and I feel the doctor-patient relationship seems especially important when the battle against cancer is shared over many years and often through multiple phases of progression and response. It’s definitely an exciting time to go into heme/onc as there are many new up and coming treatments along with endless ongoing clinical trials.
Do a lot of subspecialties in heme/onc exist? Are they traditionally additional years of dedicated fellowship training?
Great question. Those who are pursuing a career in academics tend to specialize in one area of hematology or oncology such as only treating breast or lung cancer for example. Most academic centers have faculty members for each type of cancer. Just like internal medicine, it is difficult to “know everything” and I think that’s why some are heading into the direction of just focusing on one type of cancer. A sub-specialist in an academic setting will generally spend most of their time geared towards research, clinical trials, teaching and maybe 1 or 2 days of clinic. How it typically works is you would either tailor your practice towards your specific interest or look for an opening in your area of interest which will usually be in an academic center.
For those who want to pursue a career in bone marrow transplant, additional fellowship training is required. Bone marrow transplant is an advanced fellowship which is an additional year after completing the initial 3 years of heme/onc. There are some non ACGME accredited 1 year fellowships available at top cancer centers like MD Anderson for leukemia, lymphoma, and myeloma.
Do you plan on pursuing a subspecialty?
Although I have an interest in solid tumors I will not be pursuing any subspecialty. The variety of pathology is what attracted me to this field so I would like to be a “generalist” and treat all types of cancer. If I only focused on breast or lung for example I would definitely miss seeing patients with myeloma, pancreatic, prostate, or even gynecologic cancers. My career goal is to go into private group practice and treat a variety of malignancies.
Every specialty is becoming more and more competitive to match into. Can you share with us some data on what your fellowship application looked like?
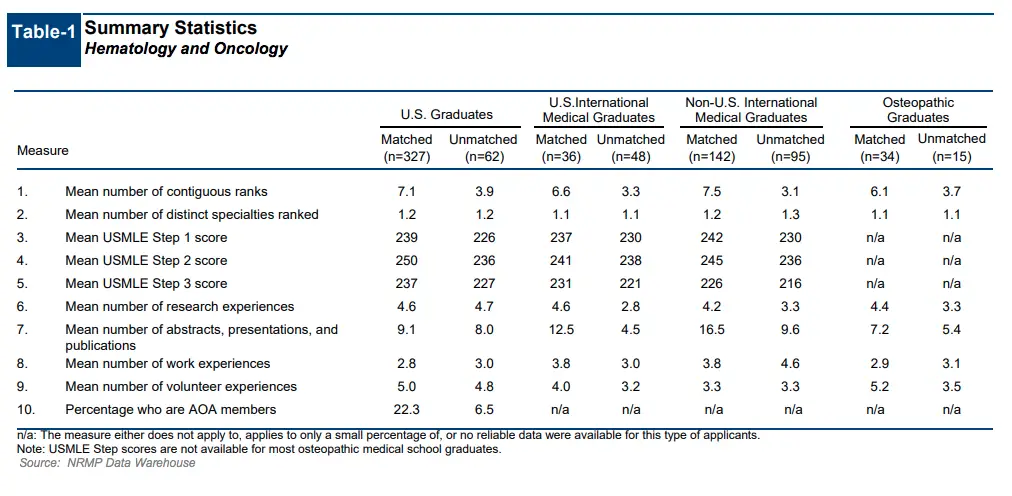
I definitely agree that most specialties continue to become more competitive each year. Here are some data for hem/onc from the 2018 NRMP fellowship match data
- 553 spots with 760 total applicants
- 73 % matched, 27% went unmatched
- US allopathic grads: 327 matched, 62 unmatched
- US IMG’s (like Caribbean med grads): 36 matched, 48 unmatched
- Non US IMGs: 142 matched, 95 unmatched
- Osteopathic: 34 matched, 15 unmatched
Below are the details on the statistics from the NRMP match data. You can see the average USMLE step scores for matched and unmatched applicants from US medical schools, IMG’s, international medical graduates, and osteopathic graduates. For instance, the average USMLE step 1 score of US, IMG, and international matched grads respectively were 239, 237, and 242.
What research did you work on during residency? Was that below, above, or an average amount of research for someone applying to heme/onc?
Research is a major component of the fellowship application (especially compared to residency). Research can be any abstracts, poster presentations, publications, or quality improvement projects. Anytime I would see a patient with a rare malignancy I would look it up to see if there have been any case reports published and if only a few have been reported, then I would use that opportunity to write up my own case report. I was taking care of a patient with a primary DLBCL (diffuse large B-cell lymphoma) of the cervix and primary pulmonary angiosarcoma (both extremely rare) and took the opportunity to write them up. They were both accepted for publication in an online oncology journal and have been presented as poster presentations at several meetings. I also worked on a case series with a gynecologic oncologist comparing patients with low grade serous ovarian cancer that was also published in an online oncology journal.
As far as poster presentations, I was able to present some of my abstracts at several meetings including the Lymphoma and Myeloma International meeting in NYC, the American College of Physicians Southeastern PA chapter meeting, the Drexel Discovery Research Day and our departments own internal medicine annual research day. I also presented an overview of the treatment guidelines for autoimmune hemolytic anemia at the Drexel Hematology journal club.
Here are some data regarding research from the 2018 NRMP fellowship match. For US allopathic grads, the average research (abstracts, presentations and publications) was 9.1 for matched and 8 for unmatched. US IMGs had 12.5 for matched and 4.5 for unmatched. Non US IMG had 16.5 matched and 9.6 unmatched. Based on this data, the more research you have, the safer you are to match. Bottom line..find time for research!!
Did you complete any quality improvement projects?
I worked on a quality improvement project with 3 other residents who were also going into heme/onc. We decided to evaluate blood transfusion utilization and cost analysis at Hahnemann University Hospital. We conducted a retrospective chart review of packed red blood cell transfusions administered at Hahnemann University Hospital during the month of May 2017. Data collected included pre-transfusion hemoglobin level, quantity of units transfused, post-transfusion hemoglobin level, the patient’s primary service, and level of care. One hundred and fifty-three charts were reviewed across all specialties and units. Twenty-one percent of blood transfusions in this period, representing 41 units of packed RBC, were determined to be inappropriately administered. Based on the figures from the ASH 2008 study, the estimated patient costs of these inappropriately administered units may be as high as $140,753. Our conclusion was that the number of blood transfusions administered during the period under review that did not follow the AABB guidelines was substantial. Stricter adherence to established evidence-based guidelines for red blood cell transfusions could represent a significant cost-saving measure.
What advice do you have for medical students interested in pursuing heme/onc?
For medical students who know they want to pursue hem/onc…more power to you! To make yourself a competitive applicant for residency, you must do well on USMLE step 1 and step 2 CK. Lower than average scores can hurt you in the long run and yes they still matter for fellowship. I would recommend setting up 1 or 2 heme/onc electives during your 4th year so you can get an idea of what it’s like to be an oncologist. Try to rotate at the outpatient clinic, as heme/onc is primarily an outpatient specialty. An inpatient or consult elective would be a misrepresentation of what the specialty is truly like.
When rotating on a hem/onc elective try to attend all of the conferences such as tumor boards and ask if you can even present a case. Feel free to ask the fellows and attendings questions on what their daily routine is like. Remember, to become a hematologist/oncologist, you must first get accepted into an internal medicine residency. So work hard and ace those boards!
What advice do you have for residents who are interested in pursuing heme/onc?
For residents interested in pursuing heme/onc, I would make sure the attendings and fellows know you’re interested from the beginning. Try to do as many rotations as you can whether it be the inpatient service, consults or outpatient clinic. The more they see you around, the more they will see that you are truly interested. I know not all residency programs will have an in-house fellowship or not have any available heme/onc rotations so I recommend scheduling an away rotation at program that has a heme/onc fellowship. This can be an “audition rotation” and might be beneficial in the long run (letters, connections, etc).
Also try to join any heme/onc interest groups and if there are none then perhaps create one! This will definitely look good on the CV.
As mentioned above, research is a vital component of the fellowship application. Try to get started early (as early as first half of intern year). Some projects will take time and you want to make sure you have enough to put on your CV come application time (towards the end of PGY-2). Ask around if any ongoing projects are available for you to join. Senior residents and fellows are good resources to ask.
Ask for letters in advance (anywhere from January-April) depending on the size of the residency program. Internal medicine program directors have to write a letter for every resident applying for fellowship so make sure to notify them early so they have ample amount of time.
How many programs did you apply to, interview at, and rank?
Hem/onc gets more competitive every year. I thought I had a decent application (also reviewed by current fellows and attendings) but I was surprised with the response I received from programs. I applied broadly to around 80 programs and only received 6 interview invites. I ranked all 6 programs and I’m thankful that I matched. I heard the safe number of interviews to have to increase your chance of matching is around 6-10 but that is variable. Some have matched with fewer and some didn’t match with 10 or even more.
I will training at East Carolina University/Vidant Medical Center in Greenville, NC. I am definitely excited for this opportunity but will miss my family and friends in Philadelphia/New Jersey.
If you had to be a component of plasma what would you be?
Hmm…I would probably be the globulins..since they are important for immune system and help protect against bacteria and viruses. I can put the boxing training to use!
If any of my readers have a follow up question where can they find you?
My instagram is @joelal_md and my email is joelalcidmd@gmail.com . Please feel free to contact me with any questions
How To Match Into Dermatology: an interview with a dermatology resident
Dermatology is one of the most competitive specialties in medicine. Today I sat down with Benny Wu who is a current dermatologyy resident at Broward Health Medical Center. He shared his journey to dermatology and some advice on how to match into derm.
Thanks for letting me pick your brain, Benny. Can you tell my readers a little bit about yourself?
It is an honor for me to share my path to Dermatology residency with your readers and followers. I am currently a PGY-2 Dermatology Resident at Broward Health Medical Center in sunny Fort Lauderdale, Florida. Before medical school, I was a figure skater for thirteen years – competed on the national and international level. In 2005, I chose to end my competitive skating career due to recurring injuries and realized it was ‘time’ to move forward with life by pursuing my second passion: medicine and science. Unfortunately, during college, I did not juggle my college coursework and figure skating very well. I had an embarrassingly low G.P.A. from the University of California, Irvine and did terribly on my MCAT. The next pivotal moment that had a direct impact on my medical career came in 2007. A medical school formerly known as the University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine, now called Rowan University School of Osteopathic Medicine (RowanSOM), offered a Master’s in Biomedical Sciences degree for students who performed poorly during college but remained interested in attending medical school. RowanSOM advised me that my chances of being accepted into their medical school would be greatly increased if I performed exceptionally well in the Master’s program and if I improved my MCAT score. I performed extremely well in the Master’s program and brought my MCAT score way up (I distinctly remembered in 2005, my Physical Science score was 5/15, but in 2008 my Physical Science score went up to 10/15). Luckily, I was accepted into RowanSOM’s D.O. program in 2008. During the Master’s program and pre-clinical years I fell in love with immunology and became invested in how the body worked from the cellular and molecular level. Because of my fascination with immunology and medical research RowanSOM invited me to complete the D.O./Ph.D. combined program in 2011. Outside of medicine, I enjoy staying physically active (running and cycling) and cooking. One of my therapeutic outlets is cooking with fresh ingredients accompanied by a glass (or several glasses) of wine!
What motivated you to pursue dermatology?
Answering the following two questions can best explain my motivation for pursuing Dermatology
(1) What interests me in Dermatology – Dermatology requires a STRONG background and fund of knowledge in Internal Medicine and its subspecialties (Infectious Disease, Rheumatology, Nephrology, Pulmonology). Response to treatment is readily appreciated and is not heavily dependent on laboratory findings. One example I share with medical students is this – imagine being able to make a clinical diagnosis and assess response to treatment independent of lab findings – of course, more often than not, a confirmatory diagnosis will require a skin biopsy (side note: there are lots of procedures in Dermatology, too!). On the other hand, as much as we would like to refute this way of thinking, the importance of outward appearance in our society, and how it impacts one’s sense of self-worth, cannot be ignored or disregarded – just ask any severe nodulocystic acne patient how he feels after a full course of Accutane – it really is life-changing!
(2) What problems do I think Dermatology faces – I emphasize the difficulties because issues in any specialty can serve as motivating factors for medical students and young attendings. In Dermatology, the pathophysiology of many skin conditions remain unclear or unknown – there is a lot of opportunities for both basic science and clinical research in Dermatology. However, the more pressing concern is the dwindling interest in complex medical Dermatology – this may be due to decreased reimbursements from insurance carriers – but I see this unique problem as an opportunity for Dermatologists-in-training to start new Dermatology fellowship programs, such as Dermatology Hospitalists. For example, severe pemphigus patients admitted for rituximab infusion – this is classically a Dermatology-driven problem that can be managed by the primary Dermatology service.
Something that impressed me about you is that how persistent you were in pursuing your desired specialty. You didn’t match into dermatology…twice. But you persisted and landed a residency position in your dream job. What did the experiences of not matching into dermatology teach you?
Not matching into Dermatology taught me the importance of focusing on my modifiable weaknesses.
After failing to match again during my intern year at Drexel, I had to ask myself two questions: (i) is Dermatology the only specialty for me? (ii) if so, what can I do to maximize my chances the third time around?
Facts are facts. I am a D.O. with average USMLE scores for Dermatology (these are not modifiable). However, my lack of publication and research experience in Dermatology was modifiable. Thus, I made a promise to myself that I would give myself one last chance – reapply to Dermatology – but this time as a Northwestern Dermatology Clinical Research Fellow.
Also, I learned how much ‘grit’ I have. Dr. Angela Duckworth’s book, “Grit: the power of passion and perseverance” discussed the importance of being ‘gritty’ especially when dealing with failures or disappointments. If you have not read this book, I urge every one of your followers to read it, especially before the interview season begins – I believe in the two equations outlined by Dr. Duckworth: talent x effort = skill; skill x effort = achievement; TALENT counts ONCE while EFFORT counts TWICE.
Why do you think you didn’t match multiple times?
I failed to match numerous times because of the following reasons:
- Did not initially consider D.O. Dermatology programs
- Did not apply broadly (limited myself geographically).
- My degree, D.O. – Dermatology is a competitive specialty even for U.S. M.D. graduates.
- Average to below-average USMLE Step 1 score (238) for matched applicants – as a D.O., a spectacular Step 1 score (>250) would have helped – but not a guarantee by any means.
- CV did not differ much between the first and second time applying.
What did you do differently the second time to improve your chances of matching? Why do you think you failed to match a second time?
I did not do anything differently the second time around – as you know, we were co-interns at the time and had limited time to add significant publications or research experiences to my CV. The only addition to my CV in the 2017 cycle was one publication – a review article on drug-induced pyoderma gangrenosum.
So you finished your required preliminary year in internal medicine and you are offered the opportunity to stay and complete a categorical three-year residency in internal medicine. Why didn’t you stay?
Do you want a fluffy answer or the real answer? ☺ I did not stay because Dermatology remained one of the few medical specialties that I could see myself doing long-term. However, I loved infectious disease as well. Like I said before, there was one modifiable ‘weakness’ in my application – Dermatology research experience. Near the end of intern year, I was offered a Dermatology Clinical Research Fellow position at Northwestern University, Feinberg School of Medicine. Privately, I told myself that if I did not match the third time around, I would complete Categorical-Medicine residency and possibly pursue Infectious Disease.
What did you do professionally after your preliminary year to improve your application while you re-applied for the third time?
Right after the Medicine-Preliminary year, I moved to Chicago and completed a Dermatology Clinical Research Fellowship at Northwestern University. Simultaneously, I entered the 2018 ERAS and NRMP and applied with new recommendation letter writers (2 from Northwestern Dermatology Faculty, 1 from University of Pennsylvania Dermatology Faculty, 1 from Drexel/Hahnemann University Hospital Medicine Residency PD) and 1 new publication (ichthyosis, X-linked) with the Northwestern Dermatology Chair, Dr. Amy Paller (https://www.ncbi.nlm.nih.gov/pubmed/28846233).
Thankfully you matched. What do you think you would have done if you didn’t match for a third time?
If I did not match, after three attempts, I would have done the following in sequential order:
- Try to secure an unfilled position through the SOAP.
- Apply to the few programs that secured extra funding for more spots or received ACGME-approval to increase program size after the NRMP Match quota deadline. Because Dermatology is a relatively small community, one advantage of doing a research fellowship at a major academic institution, such as Northwestern, is that PDs will advertise open positions on a listserv available to only Association of Professors of Dermatology Members (Dermatology PDs). Northwestern forwarded open positions to their research fellows since 2 out of 5 research fellows did not match.
- If number 1 and 2 don’t work in my favor, then I would seek out available PGY-2 Medicine Categorical positions, with the hope of specializing in Infectious Disease later down the road.
How many dermatology programs did you apply to each year? How many did you rank?
– In 2016, I applied to ~50 Dermatology Programs and 18 Medicine-Preliminary Programs. Ranked 5 Dermatology Programs (NRMP).
– In 2017, I applied to ~90 Dermatology Programs (including both Advanced ‘A’ and Physician-only ‘R’ positions). Ranked 2 Dermatology Programs (NRMP).
– In 2018, I applied to 95 Dermatology Programs (15 AOA-accredited “D.O.” programs and 80 Dermatology Programs – including both ‘A’ and ‘R’ positions). Ranked 2 AOA-accredited Dermatology Programs (NMS Match). Ranked 6 Dermatology Programs (NRMP)
What advice do you have for medical students who want to pursue dermatology?
– Read, read, and read more: highly recommend Lookingbill and Marks Dermatology textbook – this is a basic Dermatology textbook – very user-friendly.
– Approach to reading primary research articles: learn how to interpret and formulate questions as you read research articles – (i) is the study design robust – assess strengths and weaknesses (ii) any bias (iii) does it directly address the hypothesis – keep in mind that negative papers can still be valuable (iv) author financial relationship disclosure – is there a conflict of interest? Learning these skills early on will help you tremendously at audition rotations – this will quickly set you apart from other applicants – always remain inquisitive.
– Align yourself with a Dermatology mentor as soon as possible: if your school does not have a home Dermatology Department then search for a local Dermatology Society (for example, Chicago Dermatological Society [CDS] and PhillyDerm in Philadelphia, PA).
– No need to submit to only Dermatology journals: if you see a compelling case in your non-Dermatology clerkships that is Dermatology-relevant (for example, VZV reactivation in an immunocompromised patient) submit the case as a Continuing Medical Education (CME) quiz to a Family Medicine or Internal Medicine journal.
– Ask yourself these question: “is Dermatology the only specialty I see myself doing?” Remember, Dermatology has significant overlap with Rheumatology, Infectious Disease, and Family Medicine/Primary Care. By not limiting your publications to Dermatology journals, should you decide to apply to Family Medicine or Internal Medicine down the road, it will appear less likely that you ‘settled’ for another specialty.
What are important aspects of a residency application for dermatology? Is it heavily research oriented?
– Research is critical (except for a few Dermatology programs, most are academically-driven and require residents to publish annually). Many of the applicants I met on the interview trail took a year off to do research. However, a dedicated research year is not critical – instead, focus on getting 2-3 FIRST author PMID (PubMed Indexed) publications by the time ERAS is ‘due’ (typically ~ September 15)
– First authorship holds much more weight – keep in mind papers can come in a variety of flavors: case-reports, case-series, CME quizzes, and review articles.
– By taking command of your publications, this will serve you well during the interview – you may be interviewing with a faculty member who is an ‘expert’ in the topic of your research or publication(s).
Any residency interview tips specific to dermatology that you wish someone told you before you hit the interview trail?
(i) Please do not discount the value and importance of PCs! I believe that Kaiser-Los Angeles Dermatology granted me an interview because I was professional and courteous when communicating with the PC.
(ii) Compile a list of programs that you would like to receive an interview – construct a personalized letter of interest to each program – outline the reasons why that program is attractive (besides being Dermatology!) – email the letter to the PC in late September so it can be added to your file for review.
(iii) Pay attention to your speaking volume and level of engagement during the pre-interview dinner and interview day – I lived by this saying ‘loose lips sink ships.’
(iv) If you are placed on the wait-list, email the PC and ask when the interview(s) are held? – Three weeks before the interview date(s), send the PC an email reminding him/her of your interest and provide application updates, if applicable.
(v) Avoid emailing or calling the PC with general questions about the program – study and thoroughly comb through the program websites.
(vi) Only reserve emails when you have SIGNIFICANT application updates – for example, I was asked to give an oral presentation at the 2018 American Academy of Dermatology (AAD) Annual Meeting [https://www.aad.org/scientificsessions/am2018/SessionDetails.aspx?id=11492] after I certified my ERAS – after updating my programs of interest, I received an interview invite from one program several hours later.
(vii) After the interview, prepare handwritten thank you cards for the PD and PC – note: in 2018, several programs explicitly stated NO thank you cards.
(viii) Prepare written templates for the following scenarios: (a) requesting letter of recommendations (b) accepting interview invites (because rarely do Dermatology applicants reject interview invitations) (c) letter of interest – tailored to specific programs (d) post-interview thank you card (e) top choice/you are my number one letter. I have templates (Dermatology-specific) for all these scenarios – please contact me directly if you wish to see my templates.
(ix) Avoid post-interview communication with the PD, PC, and residents – unless it is for SIGNIFICANT application updates – also, no harm in sending your number one a letter of intent several weeks before the rank list is due – note: in 2018, several programs explicitly said no post-interview communications.
Here are some facts for you and my followers. In 2016, based on NRMP match rate data, dermatology was the 5th most difficult specialty to match into behind only neurosurgery, orthopedic surgery, plastic surgery, and vascular surgery. Likewise in 2016, dermatology was among the six specialties with the highest average USMLE step 1 score for applicants who matched into their preferred specialty along with neurosurgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. That average USMLE step 1 score was 250. Although I believe that high board scores shouldn’t be the only important aspect of a medical student’s residency application, it is hard to argue with objective data in that if you want to match into a highly competitive residency like dermatology you need to ace your boards. What advice do you have for medical students who want to pursue dermatology but don’t have those ultra-competitive board scores?
I scored a 238 on my USMLE Step 1 (please keep in mind that I took my Step 1 in 2011 – the passing score changed several years later). Regardless, 238 is not a strong score for Dermatology. If you scored <240 on USMLE Step 1, focus on the modifiable aspects of your application – (i) research – aim for 3 to 4 first author publications (ii) mentorship – seek out mentors as soon as possible so you have time to develop a relationship with them – this will lead to STRONG letters of recommendation (iii) research year – consider a research year (between MS III/IV) – I highly recommend the Northwestern Dermatology Pre-Doctoral Fellowship (iv) I cannot stress this enough – if you want to pursue Dermatology, remain focused on the modifiable aspects of your CV!
How did you find and develop a relationship with a mentor in dermatology?
My Ph.D. was on neutrophil biology in sepsis. Naturally, I asked myself the question “which skin conditions are driven by neutrophil dysfunction?” I found out that several neutrophil-mediated skin diseases fall under the spectrum of diseases commonly known as ‘neutrophilic dermatoses (ND).” As a fourth-year medical student, I reached out to Drs. Misha Rosenbach and Robert Micheletti from the University of Pennsylvania Dermatology (they are both Dermatology Hospitalists and have research interests in ND) – I contacted them and expressed my interest in Dermatology and ‘expertise’ in neutrophil biology. At that time, they happened to be in the process of spearheading a retrospective chart review of patients admitted with Sweet’s syndrome! Long story short, I completed two months of research with them, and they became my mentors through this process. Although I was not a University of Pennsylvania medical student, Dr. Micheletti supported my Dermatology Residency Application all three times – Dr. Micheletti emailed me on Match Monday, one hour after NRMP released the much anticipated “Did I Match?” email, and asked how I am doing and if I matched. Mentors do not have to be from your home institution. The mentor-mentee relationship takes work – take these relationships seriously but also show your ‘humanistic side’ or ‘brand of personality’ when appropriate. Remember, there are MANY ways to find and develop a relationship with a mentor – this is just one example of how I did it.
What is the biggest misconception about the field of dermatology?
The biggest misconception about Dermatology is that it is an ‘isolated’ specialty – like I mentioned before, Dermatology overlaps with many, if not all, of the Internal Medicine subspecialties – think: systemic lupus erythematosus (Rheumatology), HIV-associated dermatoses (Infectious Disease), systemic sclerosis (Rheumatology, Nephrology, Gastrointestinal, Pulmonology). There is significant overlap between all of the previously mentioned specialties – we see more multidisciplinary clinics, such as Rheumatology-Dermatology, for connective tissue disease patients with skin manifestations. Again, you do not need to limit your manuscript submissions to Dermatology journals – many internal diseases present on the skin – for instance, a CME quiz or review paper on atypical presentations of sarcoidosis can be submitted to a Pulmonology journal.
What are the strangest, most bizarre, or most unique questions you’ve been asked after people find out that you’re going into dermatology?
What people commonly say when they find out I am a Dermatology Resident is “oh, that is why you have such nice skin.” The most common question is “what should I do about X, Y, and Z (insert common COSMETIC complaints here) – because of this, I tell new people I meet that I am a Medicine Resident ☺. Also, my phone will occasionally receive pictures of rashes and bumps from my friends – I usually respond with “not interested” haha, just kidding! All jokes aside, I enjoy the question “why Dermatology?” – this question reminds me of the reasons why I chose to pursue Dermatology – and I take this opportunity to educate the public that Dermatologists are not merely ‘pimple-poppers, cyst-removers, and soft tissue injectors.’
Okay, so now the question that I’m sure you must be asked non-stop: what’s your skincare regimen?
Well, I do have pretty fabulous skin… ☺ haha. Disclaimer: ‘healthy’ skin is heavily driven by his/her genetic makeup – but evidence-based medicine suggests that sun protection and intact skin barrier are critical for optimal skin health. And of course you should not use this as medical advice. If you have skin questions or concerns you should always seek out an expert consultation with a dermatologist. This is my skin care routine:
Morning
In the shower: limit shower time to <10 min and use lukewarm, NOT HOT, water.
(a) Panoxyl 10% benzoyl peroxide (BPO) face and body wash – apply wash to my face only – prevents acne breakouts – has antibacterial and anti-inflammatory properties (BPO will whiten colored clothing so make sure you thoroughly rinse off the BPO, especially if you use colored towels).
(b) Cetaphil Gentle Cleansing Bar Soap.
Post-shower
If you are prone to eczema or dry skin – use towel to damp dry – followed by emollient (cream-based, not lotion) application – emollient will ‘lock-in’ moisture.
– Cetaphil Men’s Daily Facial Moisturizer SPF 15 – quick word about SPF – unless you have a genetic skin disease (i.e. Gorlin’s syndrome) – no need for SPF>30 – SPF and percentage of UV blocked employs a base-10 logarithmic scale – this means that an SPF of 10 blocks out 90% of UV, SPF 15 blocks out 93.3% of UV and so forth – the percentage of UV blockage basically levels off above SPF 30 – save your money and spend it on an excellent emollient, instead – see below.
– Cetaphil or CeraVe Moisturizing Cream (from tub NOT pump or squeeze bottle) – I use this to prevent moisture loss and to maintain an intact skin barrier – this is especially important for long hours in the hospital (definitely experienced this as a Preliminary-Medicine intern) – apply liberally to arms and legs.
Evening
Same as morning routine (BPO face wash) with the addition of topical retinoids – retinoids such as adapalene 0.1 or 0.3%. Retinoids are indicated for acne and pre-cancerous skin lesions, but they have also demonstrated repeatedly in several controlled studies to improve fine wrinkling, increase dermal collagen synthesis, and lighten uneven pigmentation – because of these reasons, I use adapalene 0.3% nightly – if your insurance does not cover retinoids (tretinoin, adapalene) it can be purchased over-the-counter under the brand name Differin (adapalene).
Things to avoid
Alcohol-based products (dries skin) and anything scented.

Benny Wu was born in Taipei, Taiwan and immigrated to the United States (Cupertino, California) when he was 10 years-old. Before medical school, he was a figure skater for thirteen years – competing on the national and international level. He graduated from the University of California at Irvine (Irvine, California) the same year he decided to end his competitive skating career. Before attending Rowan University School of Osteopathic Medicine, Bennybecame interested in medical research while he earned a Master’s of Biomedical Sciences from the University of Medicine and Dentistry of New Jersey. This led him to enroll in the combined D.O./Ph.D. program at Rowan University in 2009. Upon graduation from Rowan University in 2016, Bennycompleted an intense but rewarding Medicine-Preliminary internship year at Drexel/Hahnemann University Hospital in the ‘City of Brotherly Love’ (Philadelphia, PA). After his internship year, Benny fully immersed him in Dermatology clinical research by completing a Dermatology Clinical Research Fellowship at Northwestern University, Feinberg School of Medicine. Besides immunodermatology and translational research, he is passionate about mentoring medical students serious about pursuing Dermatology. Outside of Dermatology, Benny enjoys cycling, completing workouts that incorporate stability, endurance, strength, and athletic power, cooking, baking, and traveling. His next dream vacation spot is South Africa (cage dive with Great Whites). To learn more about Benny including his winding path to a dermatology residency you can follow him on Instagram at dermination_sk8r.
Interested in other specialty specific resident interviews? Check out these resident interviews and subscribe so you don’t miss out on the next blog post!
- D.O. grad who matched into OB/GYN
- Caribbean grad who matched into categorical surgery residency position
- Caribbean grad who matched into emergency medicine
- Caribbean grad who failed step 1 and matched into family medicine
- Caribbean grad who matched into internal medicine in Canada
- Caribbean grad who matched into pediatrics
- Caribbean grad who matched into PM&R
https://mykittykatz.com/what-happens-when-you-dont-match-into-residency-twice/
How To Survive 28-Hour Residency Call Shifts
In my internal medicine residency program we work 28-hour shifts while rotating through the medical and cardiac ICU every 4 days. You show up at 7am and work your usual shift and then cover all of the patients in the intensive care unit when everyone else goes home. You see new evaluations on the floors and in the emergency department and help run any codes that happen throughout the hospital. The following morning you get to leave at 11am if all the work is done and do it all over again 3 days later.
Thankfully the CCU and MICU rotations usually are only 3 week stretches at a time but it is still mentally and physically exhausting. Here are my tips to getting you and your patients through your overnight shifts alive.
Sleep (duh)
Never stand when you can sit, never sit when you can lay down, and never lay down when you can sleep. At some point you will be able to find some down time so take advantage of it when you can. I’ve found that if I can get 4 hours of sleep overnight I can somewhat function well enough the next day. 3 hours and everything takes me a little bit longer than usual. Anything less than that and I’m a zombie. Bonus points to whoever can manage to have a nap during the day before your evening call shift starts.
Pack an overnight bag
I have the same routine during every overnight shift. I claim my favorite call room with the best AC, steal an extra pillow from an unused call room, and snag two towels from the linen cart. Usually sometime around midnight or whenever there is a lull in the action I wash my face, brush my teeth, and throw on some new socks and underwear. If nothing else it makes me feel a little more refreshed and clean after being in the hospital for close to 18 hours. Of course, this plan goes sideways if I forget to bring my overnight bag. My overnight supplies consists of the following:
- Toothbrush and toothpaste
- Face wash
- Contacts/glasses
- Fresh socks
- Fresh underwear
- Advil
Meal Prep
My usual goal is to bring at least one full meal with me for my overnight shift. Sometimes that consists of a Trader Joe’s burrito or home made mac ‘n cheese while other times its simply some yogurt and a coffee K-cup. It takes minimal effort but makes a big difference when you’re tired and hungry. This way you can just be tired! Not to mention that ordering take out gets old and expensive pretty quickly.
Go home and sleep afterwards..but set an alarm
The best overnight shifts, and rarest, are ones where you get enough sleep during the night that you can just go home, take a quick nap, and have the rest of your day off to enjoy. Typically what happens is I get home by 11:15am, eat something small, and pass out. When I first started working overnight shifts as a junior resident (PGY-2) I would sleep as much as I wanted. The problem I encountered is that I would wake up at 7pm and not be able to fall back asleep until 3am. Which would be fine if I didn’t have to be back in the ICU by 7am the next morning. To avoid this sleep schedule nightmare I always set an alarm for somewhere around 3-4pm. This way I would get enough sleep to be able to function for the rest of the afternoon and also still be tired enough to have an early night. Or catch happy hour depending on the day.
How do you survive your 28-hour overnight shifts? Don’t forget to subscribe so you don’t miss my next blog post!
[button link=”https://wp.me/P31Asd-mT” icon=”envelope-o”]Subscribe![/button]
How To Prepare for Intern Year of Residency
One of the most frequently asked questions that I receive from medical students is about how to prepare for their first year of resident. It parallels one of the most common fears among medical students in that they will not be adequately prepared for day one of residency. It’s a valid concern because you will never truly be ready for intern year but if you’ve made it this far in your training then you are likely ready enough. Almost everything you learn intern year isn’t taught in medical school because you have to do actively do it to learn it. At least that’s what I thought until I came across OnlineMedEd.. It’s the only resource I’ve found that actually prepares medical students reasonably well for intern year. Again, nothing is going to make you fully prepared but this is as close as you’re gonna get.
I started using OnlineMedEd during third year of medical school
OnlineMedEd is an amazing resource with videos that help explain complicated topics that overlap real world experience with the textbook. They do an amazing job of translating all of that USMLE step 1 material into actual practical knowledge so you can look sharp on all of your third year rotations. I would watch a few before each rotation started and it showed. Dustin and the OnlineMedEd team also drill home all of the important facts that are frequently tested on step 2 CK. Sure, nothing will ever replace UWorld but OnlineMedEd gives it a run for it’s money. Start using OME early and often.
A curriculum for fourth year medical students
Your fourth year of medical school is a magical time especially after interview season is over and your rank list is finalized. You’re basically just waiting to graduate and planning your vacation to South East Asia. It is all to easy to fall into a trap of laziness and forget that you are going to be a full fledged doctor in 6 short months (well technically you’ll be an intern but a doctor nonetheless). If you dedicate yourself to the structure of OnlineMedEd during your fourth year you will have a dedicated curriculum that keeps you fresh and sharp on the wards. Sure, you’re still gonna forget a lot before intern year starts but at least OnlineMedEd will get you into some good habits.
It prepares you for intern year
My advise to all of my fourth year medical student is always the same- go home because life is too short to be spent in the hospital watching me type notes and at least one of us should see the sun today. I also tell them that the best way to be a good intern is to develop good habits while you are still in medical school. The dirty truth about residency is that you don’t need to be all that intelligent to be a good intern. You simply need to be efficient, thorough, and work hard. The sooner you develop habits that enable you to work smarter, and not harder, the better off you will be. OnlineMedEd has developed a fantastic Intern Boot Camp that helps you do exactly that. If I could do my fourth year all over again I would use the Intern Boot Camp and test out what does and does not work for me while I was still on the wards in the hospital. That way when I show up day one of residency I at least had a system that I knew worked for me. It’s like when I had to learn how to actually study in medical school- I wish I didn’t have to go through the process of figuring out what works best for me. I wish I knew how to study more efficiently back in undergrad. Likewise, take the time to learn the ropes of what it takes to be an intern while you are still a medical student.
Start studying for step 3
Ugh I know. Sorry for bringing up the USMLE’s again but you have to get it over with eventually. I’ve written extensively about when you should take USMLE Step 3 as well as how to study for USMLE step 3. If you use OnlineMedEd during your fourth year of medical school you will get a head start on it. You don’t need to use OnlineMedEd as your primary study aid but it will certainly help cement concepts in your head and make it easier for you once you start your dedicated step 3 study period as you transition from medical student to resident.
They also have great study products
Last thing I’ll mention are their study aides. The Intern Guide Book and the Quick Tables Book are great study tools for medical students. They succinctly provide you with a ton of well organized material. You have to fill in the blanks and annotate it just like any guide book. But if you are going to use OnlineMedEd then these books are essential as they go hand in hand with some of the videos. Just like any resource, the more you use it the more results you get from it!
So if you are interested in using OnlineMedEd check them out here: OnlineMedEd.
*Full disclosure: sponsored content. That being said, I only support brands that I believe in.*
The Worst Part About Being an Internal Medicine Intern
The only thing I love more than complaining about being a doctor is actually being a doctor. Intern year sucks. There’s no way around it. I wake up at 5:15am to get to the floor at 6:00am and I rarely leave at 5:00pm when my shift is scheduled to end assuming I’m not on call till 9:00pm.
I often feel my stomach growl at 9:00am and wonder why the hell I’m hungry again. Didn’t I just have breakfast? OH WAIT. I ate breakfast 4 hours ago. By noon I’ve already been at work for 6 hours.
It’s stressful. I’m constantly in situations that I don’t quite know how to handle. For instance, when my patient’s nurse walks over and tells me that my patient’s family wants to speak with the doctor. The first time it happened I kind of looked back blankly at the nurse, shrugged my shoulders and said ‘okay?’. I looked over to my senior resident inquisitively and she gave me a bleak stare back and simply said, ‘she means you…doctor’. It’s fucking terrifying.
Don’t get me wrong. I love my job. I love being better tomorrow than I was today. Sure, I would generally prefer not to look like an idiot in front of my attendings but it’s kind of inevitable. And if my pride and ego are the only things that are hurt in the process then I’m happy to learn something new. Not to mention I look dashing in that long white coat.
But the worst part of intern year so far? It isn’t the lack of sleep, or getting yelled at by a cardio fellow, or looking stupid in front of my entire team. It’s been watching my patient slowly die and not being able to do anything about it. I feel helpless. I can’t even imagine what’s going through my patient’s head.
There are literal teams of physicians working to keep my patient alive. Cardiology, cardiothoracic surgery, plastic surgery, radiology, interventional radiology, nephrology, infectious disease, gastroenterology, hematology & oncology, physical therapy, nutritionists, and the entire nursing staff (oh thank the lord for the nursing staff). And all of the ancillary staff that help us do our jobs.
When this man dies the entire hospital is going to be present for the morbidity & mortality conference. Except the one department that should have been involved from the beginning- palliative care.
Getting a palliative care consult doesn’t mean giving up on our patient. It means making the patient’s quality of life a priority.
I won’t begin to pretend to know what’s best for my patient or how to get my patient well enough to get him out of the hospital but what’s the point if we don’t make his quality of life, and his family’s quality of life, a priority.
——–
This post was originally featured on KevinMD.com
What happens when you don’t match
What happens to medical students who don’t match? Here’s what one unmatched psychiatry applicant had to say.
Thanks for letting me interview you Steven. You have a pretty unique story that my readers would love to hear about but before we delve in can you tell us a little bit about yourself? Who are you professionally? Did you go straight from undergrad to Ross? Who are you outside of the hospital?
My pleasure, Marc. I appreciate the opportunity to share my story as I feel people can learn from any experience in this process, both good and bad. I graduated from NYU in 2010 with a Bachelor of Arts in Mathematics. After graduation, I had about six months before starting with Ross University’s MERP (Medical Education Review Program) and I knew I needed to make money. So I took a job that any medical school bound person takes – working in the jewelry and diamond industry. I did mostly bookkeeping but I also prepared orders for a wholesale company that dealt with Macy’s, JcPenney, Sears, HSN, QVC, etc. It taught me a lot about dealing with large staffs and it was a nice break away from the science and math world I had spent so much time with in undergrad.
Professionally, I’m the one making jokes in the office but I focus on the patient when I’m in the room. I like to be a reason people enjoy coming to work, because they know it’ll be fun and productive. On the same token, I’m also someone who isn’t afraid to call someone out for their BS because I expect someone to do the same to me if I ever act out of line. I also am one of the first people to teach someone how things run in the office, how to order labs, do procedures, etc. Not only do people feel comfortable if it’s a peer teaching them but it helps me better my skills as well.
What specialties did you apply for? How many programs in each specialty? What was your reasoning for that number of programs?
I applied to psychiatry, internal medicine, and internal medicine-psychiatry combined. For psychiatry, I applied to 76 programs. For internal medicine, I applied to 10. And for IM-psych, I applied to all 9 programs in the country. My step scores weren’t that competitive and there are only 196 psychiatry programs in the country. I went through each program on FREIDA and checked to see if I matched their step requirements. If I did, I tried to see who the residents were. If there were zero or one Caribbean grad in all the PGY positions, then I didn’t apply as I felt that that one particular Caribbean grad may have had a connection there or had stellar scores. Plus, why would I spend money on programs that were going to outright reject me?
For IM, I applied to where I had rotated and since I could apply up to 10 for one fee, I applied to some hospitals in the NY/NJ area (which is where I’m from). And for IM-psych programs, there were only 9 so it made the most sense to apply to all of them.
How many interviews did you end up receiving? How did you feel your chances were at matching?
Formally, I received three interviews, but in total, I ranked four positions. I received 2 for psychiatry and I was taken off the waitlist for 1 IM-psych program. All of them were university-based programs. At the IM-psych program, I had mentioned that I had also applied for a psychiatry categorical position at the same place and I wanted to know if I had to come back for another interview, which I was totally willing to do. Ten minutes after that mini-interview, I had an impromptu meeting with the program director of psychiatry and she told me that she will see what the other four interviewers had to say about me from that day and she would let me know if I needed to come back or not. Two weeks later, I’m notified that she had enough to consider me for a position. Throughout the next two months prior to match day, I had received several emails about how the psychiatry program is expanding and there’s new facilities and all these wonderful things. I didn’t think I was a shoo-in but I felt that maybe I had a great shot.
So, it’s Monday, March 14th. The day applicants find out if they matched. You open the e-mail and find out that you did not obtain a residency. What’s going through your head?
Before that day, I told myself whatever happens, happens. I actually slept well the night before! I was driving in Fort Lauderdale and taking care of some errands and I happened to look at my phone. For five seconds, I was completely numb. And then it hit me. My biggest fear came true. All that work, all that money, all the stress, and for what? Nothing.
*cue Kim Kardashian ugly crying*
I can honestly say that it is one of the most devastating experiences and I would not even wish it upon an enemy. The e-mail just says “you did not match”. Not even a “good morning” or “hey girl!” Just one line that says you’re not good enough to continue in your career. After quickly doing my errands and a few snot-filled tissues later, I sped home passing several cops on the way and began on SOAP.
Most of us aren’t familiar with the SOAP, or the Supplemental Offer & Acceptance Program. Can you walk us through your experience with it? (Here’s a link to the SOAP schedule for my readers)
SOAP is a chance for unmatched applicants to apply to unfilled spots in all fields of medicine. However, this means that you will have to come up with new personal statements in the matter of hours, which is exactly what I had to do for family medicine. As Markus said in a previous posting, the website was down and no one could send in applications (because like LOL, heaven forbid the ERAS website works when it needs to).
I spoke with a friend who match into IM the year before through SOAP and she guided me through the process while she was at work. She told me to apply to the IM prelim, IM categorical, and family med programs that had the MOST open spots. I had only 45 spots to pick from and I used 5 of them on psychiatry programs that were unfilled. Then I went through family medicine and internal medicine. In retrospect, I could’ve used those 5 on family medicine or IM spots but what’s done is done.
So on Monday you found out that you didn’t match. Then during the week you went through the SOAP. Friday comes along and you find out that you didn’t SOAP into a residency. How did that feel?
By that point, I had already gone through the five stages of grief. Denial set in when I was in the car. Then anger when I was cursing at anyone on the road that was slowing me down from getting home (which is what I do on a regular basis and I’ve been trying to work on but YOU try driving on I-95 in Fort Lauderdale and Miami and tell me you don’t have road rage, but I digress…). Bargaining was SOAP. Depression set in when the 5th round of SOAP happened and I hadn’t received any offers. It continued for a week when all I saw on Facebook were my friends posting that they matched at their number one or number two choices. It wasn’t that I wasn’t happy for them. Every single one of us had a unique journey and even the people I didn’t like, I respected them enough in a professional sense to be proud that they get to continue their journey. It was more about the fact that I didn’t get to continue my journey with them.
Several months had passed and I hadn’t reached the acceptance stage of grief. It wasn’t until I went to the AAFP National Conference in Kansas City at the end of July that I had realized that I had been in the wrong field all this time. I realized within the first hour of the conference that I had such a wrong idea as to what family medicine and primary care entailed. There are so many opportunities for me as a family medicine doctor, whether it be to provide medical care for a whole family, work as a hospitalist, deal with mental health issues, or even perform procedures. After I didn’t match, I had told myself that something big was in store for me, and I finally believed it. Networking at the expo hall with the residency programs made me realize that I was a perfect fit for family medicine and that there are programs out there that WANT me. As I’m writing this, I can definitely say that I wasn’t supposed to match into psychiatry because I realized that I was meant to match into family medicine (I’m hoping). It feels good to be in that acceptance part of grief!
Why do you think you didn’t match? What were your step scores? Was your application particularly weak in any one specific area?
I had thought about not giving exact numbers here, but in all honesty, who cares? Step 1 was a 208, and step 2 CK was a 209 (yes, the EXACT passing score). Step 2 CS was a pass and everything was on the first try. I expected my Step 1 score but my CK was an absolute miracle. I had worked harder for CK than I did for step 1 and yet, I was not getting anywhere with my studying. I took a UWorld assessment two days before just to get more questions in and I had about 179. So in two days, my score JUMPED 30 points. (This is NOT a plan I recommend to ANYONE, by the way.) I know I’m a terrible test taker and that in rotations, I shined and my letters of recommendation reflected that.
In addition, I had failed one course in basic sciences, and THAT was a reason why a program didn’t take me. They were too worried that I may not pass step 3 (which I’ll go into below) and therefore, not be able to be licensed. However, my scores were good enough to get some interviews at university programs so I must have done SOMETHING right.
Do you think the fact that you attended a Caribbean medical school played a factor?
Not at all. The places I had interviewed at were very IMG friendly, as were the residencies I spoke with at the AAFP National Conference.
What do you plan to do while you wait to apply for the 2017 match?
I am currently a Clinical Teaching Fellow for Ross University. Some of my colleagues know it as “junior faculty” but teaching fellow is the formal title and you better believe I am using that on my CV. For those who don’t know what that is, my role is to act as a standardized patient for the incoming 3rd year medical students and assist other junior faculty in teaching how to handle difficult patients and certain common primary care cases, as well as how to begin to formulate an efficient style of medical interviewing. I also assist in Ross’s Ambulatory Care Competencies elective, where we prep the 4th year students for Step 2 CS by presenting cases and critiquing their notes.
Outside of Ross University, I tutor for Huntington Learning Center (which I have been doing since 4th year of med school), where I mostly do SAT/ACT math and high school subject tutoring in math as well. In addition, I’m getting my MBA in Health Services Management through Keller Graduate School of Management, which is one of the sister schools of Ross University. What’s great about that is that they have an “MD to MBA” program where I was able to get credit for 5 out of the 16 courses, so now I only need to complete 11 of them. In addition to working, I plan on taking Step 3 by the end of October. Needless to say, I only know one speed and it is full speed ahead.
How are you handling your loan debt?
Some of my loan debt could not be deferred or put into forbearance, so I have been paying that off. However, since starting grad school, I’ve been able to defer most of my loans while taking out more. Thanks, Uncle Sam!
What words of wisdom would you give to someone knowing what you know now?
Have plans A through Z ready to go from the jump. You don’t want to rely on them, but you want them ready if you have to execute them.
Go to as many networking conferences as you can. I know those things can cost money, but at the very least, go to the big ones run by the specialties to which you are applying.
But most importantly, it’s not a matter of “if” you become a resident, but rather it’s a matter of WHEN. 2016 was not my time and I realize that now. However, come 2017, I will be a better applicant and in a better frame of mind to continue on in the next chapter.
Thank you Steven for an informative and entertaining interview. I look forward to finding out where you match in 2017.