Hypertension, or high blood pressure, increases the amount of work the heart has to do. It’s like going to the gym and lifting heavier weights. Just like when you lift heavier weights at the gym to get bigger biceps, when your heart beats against a higher pressure it compensates by getting thicker. However, this compensatory mechanism can actually weaken the heart over time making it harder to perfuse the heart with blood and over time increases your risk of heart failure, heart attack, and stroke.
Some of my patients tell me, “but I feel fine”. And that’s the thing- high blood pressure is a silent killer. You can have elevated blood pressure for many years and not even ‘feel’ it. That doesn’t mean it can’t cause serious harm and increase your risk of future heart attack or stroke.
Defining Hypertension (high blood pressure)
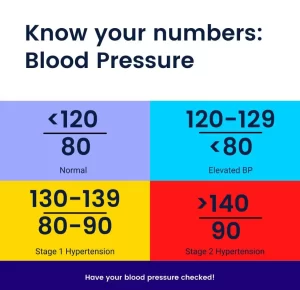
A ‘normal’ blood pressure is <120/80. That means both the systolic (top number) and diastolic (bottom number) need to be below 120 and 80, respectively. Some people have lower blood pressures and that can be completely normal. The short and skinny of it is that you want your blood pressure less than 120/80.
Below are the different stages of hypertension. How we treat blood pressure depends on your individual circumstances and medical history. It is based on robust data summarized in a the 2017 ACC/AHA (American College of Cardiology/American Heart Association) guidelines.
If you have a normal blood pressure reading (<120/80) that doesn’t mean you’re off the hook. You should still get a yearly blood pressure reading. Sometimes you just hit a certain age where your blood pressure starts to creep up a little bit. This is a good reminder that having high blood pressure, like many things in medicine, is both genetic predisposition as well as some behavioral and lifestyle choices that can impact it. Having high blood pressure doesn’t mean you did anything wrong. Some of my patients are the healthiest individuals I’ve ever met. Except that hypertension runs in their family. We will get into some behavioral and nutritional choices you can make to help bring down your blood pressure in another post.
Elevated blood pressure is 120-129/<80. Notice the different goals for the systolic and diastolic (i.e. top and bottom numbers). Essentially, if your bottom number goes above 80 you are considered hypertensive. But if your diastolic remains <80 but your systolic is 120-129 we generally recommend rechecking your blood pressure in 3-6 months. This doesn’t mean you need medications but it does mean that we want to ensure you don’t develop high blood pressure. It’s also another chance to make some positive lifestyle habits and nutritional choices that can pay off over time. As many of my patients can attest, one of my favorite sayings is that many of the choices we make today can pay off over time. Like building a strong retirement fund with a good interest rate. In contrast, ignoring high blood pressure is like having bad debt. Either way- the interest is going to compound. So it’s always better to know if you have high blood pressure than to ignore it.
Stage 1 hypertension is either a systolic between 130-139 or a diastolic between 80-89. This is where working with your physician is important. In patients at higher risk of heart disease, like those who already have clinical evidence of atherosclerotic cardiovascular disease (i.e. prior stroke, heart attack) we often will initiate both lifestyle modifications and treatment with blood pressure medications. If you are a low risk patient we can consider lifestyle modifications alone and rechecking your blood pressure in a few months. If lifestyle modifications do the trick and bring down your blood pressure we can avoid using medications. But if you are doing all the right things and your blood pressure won’t budge then you likely will require medications to lower your blood pressure. Regardless, patients with stage 1 hypertension should be reassessed in 1 month.
Stage 2 hypertension is either a systolic >140 or a diastolic >90. In these patients we often jump to use medications while also initiating lifestyle modifications because the degree that lifestyle modifications will impact your blood pressure likely won’t be enough. Just like how you wouldn’t ignore a leak under your sink you should also not ignore high blood pressure-both will cause damage over time. This is where talking with your physician is important because not all patients are alike. If you want to avoid using medications I certainly don’t think it’s unreasonable to hold off if you are right on the borderline of stage 1 and stage 2 of hypertension as long as we have a plan in place and you continue to follow up. However, a blood pressure of 142/88 for instance is very different than a blood pressure of 180/100. For latter blood pressure (i.e. 180/100) would likely require initiation of medications right away. All patients with stage 2 hypertension should be also reassessed in 1 month (just like those with stage 1 hypertension).
The more uncontrolled your blood pressure is and the greater the period of time that it remains uncontrolled the greater your risk of heart disease (e.g. heart attack, stroke). Just because you have high blood pressure doesn’t mean you will have a heart attack and just because we treat your high blood pressure doesn’t mean you won’t. It’s all about decreasing that intrinsic risk.
Why you should check your blood pressure at home
In my clinical practice I like when my patients take their blood pressure at home for a few reasons. First, if you’ve ever been to a doctor’s office you know it can be a little anxiety inducing. That’s why I never make drastic changes based on a single blood pressure reading. Some patients can have white coat hypertension– when the blood pressure readings at your doctor’s office are always elevated but when you take them at home they are normal. These patients don’t need to be treated for high blood pressure!
Second, you can only go the doctor’s office so many times. Taking your blood pressure at home gives us additional data points to use to estimate your average blood pressure. Generally, I care the most about the your blood pressure trend. Let’s look at two patients as an example. ‘Patient 1’ consistently gets systolic blood pressure readings in the 140-150’s but occasionally gets a systolic blood pressure of 118. ‘Patient 2’ on the other hand gets consistent systolic blood pressure readings in the 120’s but occasionally gets a systolic blood pressure reading in the 140’s. In both patients I won’t ignore the occasionally high or low reading but I care more about where your blood pressure average tends to be.
How to take your blood pressure at home
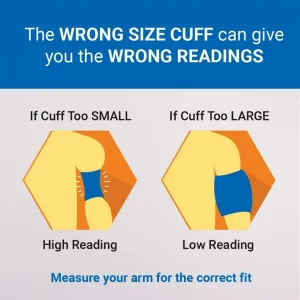
Type of blood pressure cuff
How to actually measure your blood pressure
If you don’t like reading I made a short TikTok video explaining how to actually check your blood pressure (shown below). The following tips aren’t to torture you- they are so we get accurate readings. The important things to remember are:
- Blood pressure cuff should be bare to skin (not over clothing)
- Keep your arm supported (don’t elevate it in the air)
- Keep your feet flat on the ground
- Don’t cross your legs
- 30 minutes before taking your blood pressure do not smoke, drink caffeine, or exercise (life hack- take it first thing in the morning before your first cup of coffee or if you smoke before your first cigarette)
- You can repeat the reading after waiting 5 minutes. I typically tell patients to take it once in the morning and once in the evening
- WRITE DOWN YOUR READINGS IN YOUR PHONE OR NOTE PAD AND BRING THE READINGS TO YOUR NEXT DOCTOR’S VISIT
Don’t forget to bring your readings to your next doctor’s appointment
Every day after work when I leave the hospital I put my hospital identification card in my car. That way I don’t have to remember to take it with me to work the next day. Because believe me there’s nothing worse than getting to work and having to turn around and drive home to pick up your ID badge. Similarly, remove road blocks from bringing your blood pressure readings to your next doctor’s appointment by putting the information directly into your phone. This way you don’t have to remember to bring the notepad you’ve been writing your blood pressure readings in. If you choose to do it the old fashioned way with pen and paper that is perfectly fine. Just remember to bring it to your next visit. Remember to document both the top and bottom number in addition to your heart rate. Lastly, please do not rely on your memory to serve as a blood pressure log. I want to know what blood pressure readings you are getting at home and not just that it was ‘high’ or ‘normal’.
If you found this helpful then: